Global Patient Safety Forum
The GPSF is a convening alliance with a mission to save lives, save money, and build value in the community it serves. The Forum was expressly founded to make available important content that the collaborators want to share more broadly. This website is not intended to compete with any other initiative and will meet its objectives if collaborators and those interested in the topics share the information with their communities. There is no financial requirement of users of the site.
Global Innovators Network
We are a global network of leaders from academia, industry, government, NGOs, philanthropy, and faith-based organizations who are collaborating on best practices in leadership of innovation. Spawned to meet the global needs of innovators in healthcare and patient safety, our work has expanded to multiple sectors with a focus on mentorship and development of great leaders. There is no specific commercial purpose of this website and no required financial relationship between the collaborators. The information available through this website is entirely free.
- Featured Leaders
- Global Patient Safety Teams
- Global Summits & Programs
- Best Practices Collaboration
- Governance Leaders Program
- CareUniversity & CareMoms
- Performance Impact Programs
- Media & Documentaries
|
|
Thomas Zeltner, MD Read bio... Thomas Zeltner, MD, is an international expert leader in public health and health system development. He was a 2010 Fellow of the Advanced Leadership Initiative of Harvard University. He is co-founder of the Global Patient Safety Forum, a convening organization of the world's leading patient safety organizations, and a Managing Editor of the Journal of Patient Safety. He advises international organizations and national governments in health policies and health policy reforms. He has served as Special Envoy in financing for WHO. In this capacity, he advised the Director General of WHO on the identification of an improved financing framework for the Organization. He served as Special Envoy of WHO, advising the Director General in critical areas of the current reform of this UN agency (how to cooperate with non-State actors such as NGOs and organizations in the private sector without compromising WHO's integrity, and how to better align WHO's priorities with the resources available to finance them). He is a member of the Global Agenda Council on Digital Health of the World Economic Forum (WEF).
Dr. Zeltner is president of Blood Transfusion CRS Switzerland, the organization in charge of securing Switzerland's provision with blood and blood products. He is a board member of the Swiss Academies of Arts and Sciences and President of Science-et-Cité. Since 1992, he has been Professor of Public Health at the University of Bern, Switzerland. From 1991 to 2009, Dr. Zeltner was the Director-General of the Federal Office of Public Health of Switzerland, the National Health and Public Health Authority and Secretary of State for Health. In this function he was a key actor in Swiss health policy and represented Switzerland in many international health organizations. He was graduated with an MD and a master's degree in law from the University of Bern. He holds a specialist degree in human pathology and forensic medicine. Hide bio |
|
See video clip Close Video Clip |
|
|
C. R. Denham, II, MD Read bio... Dr. Denham launched the Global Patient Safety Forum with other global leaders in healthcare including Dr. Thomas Zeltner, the former health minister of Switzerland and other quality leaders from the Mayo Clinic, Cleveland Clinic, and Harvard affiliated hospitals who all are asked to serve audiences outside of the United States.
Denham and the other leaders from clinical, operational, administrative, legal, human resources, and policy areas have convened to communicate very important patient safety information that crosses all borders. As a practicing radiotherapist in the U.S., Dr. Denham had learned the critical role of education when it came to radiation safety for caregivers and patients. The founders of the Global Patient Safety Forum seek to meet the needs of both industrialized nations and emerging nations as is addressed by the work in the 5 Rights of Imaging found on this website. Dr. Denham has taught innovation R&D and performance improvement of products, services, and technologies both in the US and abroad. Although he started his career as a doctor in private practice, his work in quality with the Institute for Healthcare Improvement, National Quality Forum, and Premier Innovation Institute prompted invitations to join academic work in performance improvement. As a Professor of Health Engineering adjunct faculty at the at the Mayo Clinic medical school with duel teaching appointments at the Harvard schools of public health and school of medicine, he has worked with educators and researchers from across the globe. After serving as an associate editor with a wide following of his articles, he was appointed the Editor and Chief of the Journal of Patient Safety and has produced more than 100 works including peer reviewed articles and multimedia productions. Through a national R&D testbed in the US, his not for profit organization is in its 10th year of leading more than 100 international web programs. Two feature length movies globally broadcasted through Discovery Europe and international partners have brought quality improvement information to caregivers and consumers. The films have featured the critical work led and supported by the World Health Organization in Geneva. The purpose of the Global Patient Safety Forum will be to continue to serve international audiences with information and media that may have been produced in the United States and been refined for global audiences. One of the latest areas of focus by Denham and the GPSF team are in pre-hospital care of the most common causes of death that can be delivered by non-clinical family members and the public before emergency services arrives. The Medical Tactical program developed by the group will be addressing the leading causes of death to children, youth, and adults in the workforce years. A second research area is in the domain of healthcare fraud including that which may be undertaken by caregivers, administrators, academics, or journalists in the healthcare and life sciences sectors. Trust is at an all-time low in caregivers, patients, and young faculty who are battling for their very families lives. The frontline research involves active reputational and rescue initiatives of the careers of caregivers in multiple communities. The goal of Dr. Denham and the leadership team are to address systems issues and especially insider and outsider threats that can be minimized through prevention, preparedness, protection, and performance improvement practices. Hide bio |
|
See video clip Close Video Clip |
|
|
Clayton Christensen, MBA DBA Read bio... Clayton Christensen is the Kim B. Clark Professor of Business Administration at Harvard Business School. He is regarded as one of the world's top experts on innovation and growth. He holds a B.A. with highest honors in economics from Brigham Young University (1975), and an M.Phil. in applied econometrics from Oxford University (1977), where he studied as a Rhodes Scholar. He received an MBA with High Distinction from the Harvard Business School in 1979, graduating as a George F. Baker Scholar. In 1982 Professor Christensen was named a White House Fellow, and served through 1983 as assistant to U.S. Transportation Secretaries Drew Lewis and Elizabeth Dole. He was awarded his DBA from the Harvard Business School in 1992. Professor Christensen became a faculty member there in 1992, and was awarded a full professorship with tenure in 1998. He holds five honorary doctorates and an honorary chaired professorship at the Tsinghua University in Taiwan.
Christensen has served as a director of many companies, and has advised the executives of scores of the world's major corporations. Christensen is also an experienced entrepreneur, having started four successful companies. Prior to joining the HBS faculty, in 1984 he and three MIT professors founded CPS Technologies, which has become a leading developer and manufacturer of products from high-technology materials. Professor Christensen is the best-selling author of eight books and more than a hundred articles. The Innovator's Dilemma received the Global Business Book Award as the best business book of the year (1997); and in 2011 The Economist named it as one of the six most important books about business ever written. Professor Christensen was featured in the Discovery Channel documentary Surfing the Healthcare Tsunami: Bring Your Best Board along with a number of others participating in the Innovators Network as he has been a tireless champion for values grounded leadership. Hide bio |
|
See video clip Close Video Clip |
|
|
Ann Christensen, MBA Read bio... Ann Christensen directs the overall strategic and operational development of the Institute and oversees its rapidly growing research programs. She also works closely with the Board of Directors to enhance the Institute’s impact and strengthen its strategic partnerships and resources. Prior to joining the Institute, she worked at Huntsman Gay Global Capital, a private equity firm focused on middle-market companies. She previously also worked at Deloitte Consulting in New York City, where she was instrumental in establishing the Growth & Innovation practice by drawing on the theories of disruptive innovation to help clients create new growth businesses. Ann led projects for clients in a number of industries, including: pharmaceutical, biotech, telecommunications, travel, professional services, and insurance. She has also spent time as a strategic analyst for Elan Pharmaceuticals, an Irish biotechnology company. Ann earned a BA from Duke University, where she studied the political economies of developing nations, and an MBA from the Harvard Business School. See more at: http://www.christenseninstitute.org/our-team/ann-christensen/#sthash.DT0qxM28.dpuf Hide bio |
|
|
Franck Guilloteau Read bio... During his 20 years with HCC Corporation, Franck Guilloteau led multiple projects, spanning industry segments from aerospace and consumer products to software and fitness. As former Chief Technology Officer, Mr. Guilloteau took the lead role in developing Software as a Service (SaaS) offerings and knowledge management systems used by HCC's global partners, while keeping HCC on the leading edge of technological advancements in multimedia, IT, e-commerce, and product development. Mr. Guilloteau was Director of TMIT, a non-profit medical research organization dedicated to driving adoption of high-impact clinical solutions in patient safety and healthcare performance improvement. He led operations at TMIT in Austin, TX, and coordinated activities related to TMIT's research and scholarship programs. He also led the Greenlight Program, a national effort focused on building business cases and clinico-economic models to "green-light" quality and patient safety investments. Over the last several years, Greenlight has targeted healthcare-acquired infections, as well as medical imaging research on the over-use, misuse, and underuse of imaging studies using the "5 Rights of Imaging®" as a framework. He also led the team involved in development of SpeakerLink®, a website where healthcare organizations can find and engage patient advocates focused on improving caring in their communities. He was involved in the development of the Computerize Prescriber Order Entry (CPOE) Simulator used by The Leapfrog Group to measure effectiveness of deployed HIT systems in hospitals and ambulatory settings. In addition to his expertise in engineering and product development, he has lived in several countries, which provides him with a unique multicultural perspective as well as fluency in three languages. Mr. Guilloteau received a mechanical engineering degree from the University of Texas at Austin, and subsequently pursued a fellowship in Biomedical Engineering with a minor in product development. Hide bio |
|
See video clip Close Video Clip |
|
|
Jeanne M. Huddleston, MD, FACP, FHM Read bio... Jeanne M. Huddleston, MD, FACP, FHM, is a past President of the Society of Hospital Medicine, the founder of Hospital Medicine and past Program Director of the Hospital Medicine Fellowship at Mayo Clinic, Rochester, MN. She is the former Chairperson of Mayo Clinic's Mortality Review Subcommittee, a multi-disciplinary group of providers that review every death in search of where the health care delivery system may have failed the providers and/or the patient. She received her MD degree in 1993 from the College of Human Medicine, Michigan State University. She completed her residency in internal medicine and advanced general medicine fellowship at Mayo Clinic. Dr. Huddleston is a Harvard Macy Scholar (both in the Physician Educator and the Leadership Programs) and alumnus of the Health Forum/AHA Patient Safety Leadership Fellowship. Dr. Huddleston has received Masters' Degrees in both Clinical Research and Industrial Engineering. This education equipped her scholarly translation of systems engineering to health care delivery in an effort to improve the value of the healthcare experience for patients, their families and the providers through her work in mortality reviews and patient threat safety. She has led the mortality review program of more than 10,000 patients that has led to a dramatic impact on the quality of care there and she now leads an international collaborative and has engaged multiple hospitals that are putting her innovations to work. Hide bio |
|
|
J. Michael Henderson, MD Read bio... J. Michael Henderson, MD, is Chief Medical Officer at the University of Mississippi Medical Center and the former Chief Quality Officer at the Cleveland Clinic. His interest in quality was initially triggered in the surgical arena, implementing standardized approaches to preoperative processes, and becoming a champion for the National Surgical Quality Improvement Program of the American College of Surgeons. In 2005, he embarked on an expansion of Quality and Patient Safety for the Cleveland Clinic. His leadership support in establishing the Quality and Patient Safety Institute has provided a central coordinating quality focus across the more than 20,000 employees. This Institute collaborates with the clinical and support departments to align quality outcomes and patient safety into daily practice for the entire healthcare team. The focus of this work is to make daily practice patient-centric, clinically relevant, operationally effective, regulatory compliant, and academically appealing. Hide bio |
|
See video clip Close Video Clip |
|
|
Nancy Conrad Read bio... Nancy Conrad created the Conrad Foundation in 2008 to energize and engage students in science and technology through unique entrepreneurial opportunities. By enabling young minds to connect education, innovation, and entrepreneurship, the Foundation helps provide a bold platform for enriching the innovative workforce of the future. Ms. Conrad’s interest in patient safety began as a result of the death of her husband, astronaut Charles "Pete" Conrad. On July 8, 1999, while motorcycling, Pete ran off the road and crashed. His injuries were first thought to be minor, but he died from internal bleeding about six hours later. Ms. Conrad’s compelling story serves to personalize the need for patients and their families to take responsibility for their care, as well as to highlight the need for systemic changes in the quality of care. Ms. Conrad was co-founder and co-chairman of fundraising of the Community Emergency Healthcare Initiative. This program was designed to measurably affect preventable injury and death occurring in emergency departments. She established the Pete Conrad National Patient Safety Award to recognize global contributors in patient safety. Hide bio |
|
See video clip Close Video Clip |
|
|
Christopher R. Peabody, MD, MPH Read bio... Christopher R. Peabody, MD, MPH is a practicing Emergency Physician in California and Clinical Instructor at the University of California, San Francisco. He is also the Director of the UCSF Acute Care Innovation Center, an initiative of the UCSF Department of Emergency Medicine, which develops novel ways to deliver Emergency and Acute Care reliably and safely by developing new technology and validating best practices. He has a strong commitment to public service and healthcare delivery to vulnerable populations. Dr. Peabody completed his residency at one of the busiest safety-net hospitals in the country, Los Angeles County Hospital, and was the Chief Resident in Emergency Medicine at the University of Southern California. He attended medical school at the University of California San Francisco, and completed an MPH at Harvard University on a Zuckerman Fellowship. Dr. Peabody's current interests lie in quality improvement and patient safety, especially related to underserved populations. He has extensive experience in emergency care and disaster response internationally, having served in Haiti and China. He is a member of the content leadership development team for CareUniversity and applies his expertise in emergency care, public health, and international healthcare performance improvement to meeting the needs of both consumers and caregivers. Hide bio |
|
|
Gladstone C. McDowell, II, MD Read bio... Dr. McDowell is a Director of TMIT and on the Global Innovations Team of the Global Patient Safety Forum, and is the Medical Director of Integrated Pain Solutions. He is a trained specialist in urology, urologic oncology, anesthesiology, pain management, and patient safety. He has served as an instructor at The University of Ohio for both the Department of Urology and the Department of Surgery. He has also served as the Director of Sabine Urology Outpatient Clinic and the Chief of Urology at Brackenridge Hospital in Austin, TX. Dr. McDowell has been involved in breakthrough research at the Gynecology Clinic of the Southwest Foundation for Research and Development, and at the Department of Cell Biology at The University of Texas' M.D. Anderson Cancer Center. Hide bio |
|
See video clip Close Video Clip |
|
|
Stephen J. Swensen, MD, MMM, FACR Read bio... Stephen J. Swensen, MD, MMM, FACR, is the former Medical Director for Leadership and Organization Development. He has served as the Director for Quality and Associate Dean for Value. He is Professor in the Mayo Clinic College of Medicine. Under his leadership the Quality Academy and the Value Creation System were established. In these programs, several thousand staff are trained each year. There are more than 13,000 certified Bronze, Silver, and Gold Quality Fellows.
Dr. Swensen chaired the Department of Radiology from 1998-2006. His leadership team used Lean-Sigma and Baldrige methods to improve the value of care for patients provided by 1,200 staff, who performed more than one million exams annually. During his tenure the department was recognized as the #1 radiology practice in the country (Medical Imaging) and the most patient-centered (Diagnostic Imaging). He holds a Master of Medical Management degree from Carnegie Mellon University's Heinz School of Public Policy and Management. He received his MD from the University of Wisconsin. His residency training was at Mayo Clinic and his Thoracic Radiology Fellowship at Harvard Medical School, Brigham and Women's Hospital. Dr. Swensen is a member of the Institute for Healthcare Improvement faculty. He served as the healthcare member of The Conference Board’s U.S. Quality Council. He is past President of two international societies, the Fleischner Society and the Society of Thoracic Radiology. He chaired the American College of Radiology's Quality Metrics Committee and led the RSNA's Continuous Quality Improvement Initiative. He is a member of the AAMC Integrating Quality Steering Committee. He founded the Big Sky Quality Roundtable and the Keystone Quality Officer Group, and co-founded the Sun Valley Assembly. He has been Principal Investigator of three NIH grants related to lung cancer screening with CT and diffuse infiltrative lung disease. He has authored two books and more than 130 peer-reviewed articles. Hide bio |
|
See video clip Close Video Clip |
|
|
Pablo Pulido, MD Read bio... Dr. Pulido is a Venezuelan physician with specialties in cardiology and internal medicine. He is currently the Executive Director of the PanAmerican Federation of Associations of Medical Schools, Caracas, and also a 2009 Fellow of the Harvard Advanced Leadership Initiative. He has participated in the dynamic evolution of a leading technical university in Caracas. In Public Policy, as Minister of Health and Social Welfare, he initiated the restructuring of the Ministry and the decentralization of operations towards the Venezuelan States. In International Medical Education, as the Executive Director of the PanAmerican Federation of Associations of Medical School, PAFAMS, he has focused on the modernization and involvement of medical schools in healthcare reforms using the new information technology, management, and curricular updating as basic instruments. Hide bio |
|
|
Samir Toubassy, MBA Read bio... Samir Toubassy, MBA, is currently CEO of Global Education Partners; an Advanced Leadership Senior Fellow at Harvard; and a former President of The Olayan Development Corporation and former Group Vice President. The Olayan Group is one of the largest privately-held global business conglomerates through its Riyadh, Athens, London, and New York offices. After working with The Olayan Group for 30 years, Mr. Toubassy continues to serve as a Senior Advisor and member of the Executive Committee. He served for several years as a member of Coca-Cola Beverages; Coca-Cola Hellenic; and Frigoglass group of companies; and as a Senior Advisor to Crédit Suisse and a member of the Advisory Board for Europe, the Middle East, and Africa. Mr. Toubassy is a Trustee and Vice Chairman of the Nomination and Governance Committee of the Thunderbird School of Global Management. He is a member of the Advisory Board for the Churchill Archives Centre, Churchill College, Cambridge University; and a member of the Dean's Council, John F. Kennedy School of Government at Harvard University. He also serves on the board of the American Near East Refugee Aid (ANERA), a voluntary organization working for the Middle East. For the past 12 years, Mr. Toubassy has been actively involved in the World Economic Forum. Prior to joining The Olayan Group, Mr. Toubassy worked with the Ford Foundation in public administration reform in the Middle East. He also worked for the American University of Beirut and the University of California system-wide administrations. Mr. Toubassy holds a bachelor's degree in Business Administration from the American University of Beirut, and an MBA from Golden Gate University in San Francisco. Hide bio |
|
|
David C. Classen, MD, MS Read bio... David C. Classen, MD, MS, is Chief Medical Information Officer (CMIO) at Pascal Metrics in Washington, DC. Previously, he was Chief Medical Officer (CMO) and a Vice Senior Partner at CSC, and leads led CSC's safety and quality of healthcare initiatives. Dr. Classen is also an Associate Professor of Medicine at the University of Utah and an Active Consultant in Infectious Diseases at The University of Utah School of Medicine in Salt Lake City, Utah. He received his medical degree from the University of Virginia School of Medicine and a Master's of Science degree in medical informatics from the University of Utah School of Medicine. He served as Chief Medical Resident at the University of Connecticut. He is board-certified in Internal Medicine and Infectious Diseases. He was the chair of Intermountain Health Cares Clinical Quality Committee for Drug Use and Evaluation, and was the initial developer of patient safety research and patient safety programs at Intermountain Healthcare. In addition, he developed, implemented, and evaluated a CPOE program at LDS Hospital that significantly improved the safety of medication use. Hide bio |
|
See video clip Close Video Clip |
|
|
Edward Kelley, PhD Read bio... Edward Kelley, PhD, currently serves as Coordinator and Head of Strategic Programmes for WHO Patient Safety. His responsibilities include the development of new programs and partnerships; oversight of WHO Patient Safety presence in London and Baltimore; and leadership on several key programmes within WHO Patient Safety. Prior to joining WHO, Dr. Kelley directed the only ongoing national examination of healthcare quality and disparities in the United States as the Director of the U.S. National Healthcare Reports for the U.S. Department of Health and Human Services in the Agency for Healthcare Research and Quality (AHRQ). These reports track levels and changes in quality of care for the American healthcare system at the national and state level, as well as disparities in quality and access across priority populations. Dr. Kelley also directed the 28-country Health Care Quality Improvement (HCQI) Project of the Organization of Economic Cooperation and Development. Previously, Dr. Kelley served as a Quality Assurance Advisor for URC’s Quality and Performance Institute while also serving as Scientist in the Operations Research Division for the USAID-sponsored Quality Assurance Project (QAP) and Partnerships for Health Reform Project Plus (PHRPlus). In these capacities he worked for 10 years in West and North Africa and Latin America, directing research on the Integrated Management of Childhood Illness in Niger. Hide bio |
|
See video clip Close Video Clip |
|
|
Hilary J. Schmidt, PhD Read bio... Hilary J. Schmidt, PhD, is an advanced education expert with extensive experience applying principles and research from the behavioral sciences to the design of highly effective health sciences education. She has a PhD in psychology from the University of Pennsylvania and has dedicated her professional life to translating research on how people learn into best practices for teaching, learning and assessment. She has worked in both academia (17 years) and in the Pharmaceutical industry (9 years) has expertise in cognitive psychology, education research, instructional design and outcomes assessment. In academia, Dr. Schmidt founded and lead three centers for teaching and learning at NY area medical Schools including Columbia University Medical Center, SUNY-Downstate, and UMDNJ-Newark. She has authored books on study and testing skills, for medical students, and has published extensively in the field of medical education. In industry, at Sanofi pharmaceuticals she provided strategic leadership to the groups responsible for Independent Medical Education Grants, Investigator Initiated Research Trials, Transparency, and Medical Affairs Compliance Training. She is a member of the Alliance for Continuing Education in the Health Professions (ACEHP) and served as the Chair of the Industry Alliance for Continuing Education in the Health Professions from 2011-13. She was a nominated member of the AMA Task Force on Industry Provider Collaboration in CME and served a s the Annual Meeting Chair for that organization in 2012. She is the recipient of the ACEHP’s Presidents Award 2013 for service provided to the organization. She is a frequent invited speaker at medical education conferences. She recently co-founded (2014) the Calibre Institute for Quality Medical Education whose mission is to "Leverage Best-in-Class Education to Improve Patient-Care and Lower Healthcare Costs". Hide bio |
|
|
Mace Wolf Read bio... Mace Wolf began his career as the creator of the first Windows based practice management systems for medicine in 1992. These solutions were being deployed at several university hospitals and large physician practices including those of Temple University and the University of Arizona by 1994. Mace’s EDI expertise had him creating the singular EDI client software and protocols for Blue Cross/Blue Shield of Northern California by 1995. He then obtained several database patents pertinent to large datasets and analytics. Today, Mace is focused on the convergence of risk management and healthcare delivery. Current customers include over 30 Medicare Advantage plans, most of which are focused on end-of-life care for dual eligibles in addition to several physician groups, ten PACE companies, a hospice, licensed homecare agencies, and a vision plan. At Cognify, Mace is responsible for everything from financial and claims adjudication systems to electronic health records, enrollment, medication management, logistics systems, and government mandated data collection, submission, compliance and analytics. Mace is also the developer of a unique fda approved dosage management system for an international pharmaceutical company and is also the inventor of several privacy management patents pending. He is a leader of integration and the system development serving CareUniversity and its initiatives that serve both consumers and caregivers. He spends his life at the leading edge of healthcare delivery, quality, risk management, and patient safety. Hide bio |
|
|
Gregory H. Botz, MD, FCCM Read bio... Adjunct Clinical Associate Professor, Department of Anesthesiology, Stanford University School of Medicine Gregory H. Botz, MD, FCCM, is a Professor of Anesthesiology and Critical Care at The University of Texas MD Anderson Cancer Center. He received his medical degree from The George Washington University School of Medicine in Washington, DC. He completed an internship in internal medicine at Huntington Memorial Hospital, and then completed an anesthesiology residency and critical care medicine fellowship at Stanford University in California. He has served on the faculty at Duke University School of Medicine, and is an Adjunct Clinical Associate Professor of Anesthesia at Stanford University School of Medicine. Dr. Botz is a 2004 graduate of the Intermountain Healthcare Advanced Training Program in Health Care Delivery Improvement. He is a member of the steering committee and faculty for the MD Anderson Clinical Safety and Effectiveness training program, and a Charter Fellow in Clinical Safety and Effectiveness for the UT System. He has served as the University of Texas Chancellor's Health Fellow in Quality of Care and Patient Safety. Dr. Botz is currently the medical director of the Simulation Center and Code Blue Team Operations. He was previously medical director of the ICU, Transfer Center, Acute Care Training Center, and the Medical Emergency Rapid Intervention Team. As a clinician-educator, Dr. Botz serves as regional faculty for the American Heart Association Emergency Cardiovascular Care training programs, and he is a national consultant for the Society of Critical Care Medicine training programs. He was a senior editor for the American Board of Anesthesiology Joint Council on Anesthesiology Examinations, program director for the UTHSC-Houston Anesthesiology Critical Care Medicine Fellowship, and a member of The University of Texas System Health Care Components ICU Quality Improvement Collaborative. He has participated in SCCM education programs in collaboration with the Japanese Society of Intensive Care Medicine, the Saudi Critical Care Society, the Indian Society of Critical Care Medicine, and the Association of Intensive Medicine in Brazil (AMIB). Dr. Botz has collaborated with the Saudi Critical Care Society and the Saudi Commission for Health Specialties in the creation of a critical care medicine residency program, and served as an external board examiner for the Saudi Critical Care Medicine Board Examinations. Dr. Botz is the content leader for the Global Med Tac Training Certification program focused on lifesaving bystander care for the leading causes of preventable death in children, youth, and adults in workforce years. Hide bio |
|
See video clip Close Video Clip |
|
|
William Adcox, MBA Read bio... With 37 years in municipal and campus policing, William H. Adcox serves as the Chief of Police and CSO at The University of Texas MD Anderson Cancer Center and The University of Texas Health Science Center. Chief Adcox holds an MBA degree from UTEP and is a graduate of the PERF's Senior Management Institute for Police and the Wharton School ASIS Program for Security Executives. He is the recipient of the IACLEA's 2013 Award for Administrative Excellence and was named by Security Magazine as one of the "Most Influential People in Security 2013." The agency received the IHSS Foundation's prestigious 2015 Lindberg Bell Distinguished Program Award. Nationally, Chief Adcox received the Campus Safety 2015 Director of the Year Award in Healthcare; and locally he received the Texas Police Chiefs Association's 2015 Leadership Award. He is recognized as a pioneer of the discipline of Threat Safety Science which integrates patient and caregiver safety into an Institutional Health System model. Hide bio |
|
|
Vicki King, MSCJ Read bio... Vicki King, MSCJ is the Assistant Chief of Police with the University of Texas Police at Houston. During her 30-year career, Vicki served 27 years with the Houston Police Department, rising to the rank of Assistant Chief and earning a master’s degree in Criminal Justice. As Chief of Detectives, Tactical Support Commander, and Director of Forensic Services, she oversaw some of HPD’s highest-profile cases, including serial homicides, corruption, domestic violence, sexual assaults, and gangland slayings. After retiring from HPD, Inspector King served as an emissary to the Saudi Royal family; as an adjunct professor for the University of Houston system; and as Chief of Police for the City of La Marque. MD Anderson and UT-Health recruited Inspector King to head up their Threat Assessment Unit. In her new role, Inspector King works with multidisciplinary teams to identify and mitigate risks. Hide bio |
|
|
John J. Nance, JD Read bio... One of the key thought leaders to emerge in American healthcare in the past decade, John J. Nance brings a rich and varied professional background to the task of helping doctors, administrators, boards, and front-line staff alike survive and prosper during the most profoundly challenging upheaval in the history of modern medicine. Having helped pioneer the renaissance in patient safety as one of the founders of the National Patient Safety Foundation in 1997, his efforts (and healthcare publications) are dedicated to reforming American healthcare from a reactive cottage industry to an effective and safe system of prevention and wellness. A lawyer, Air Force and airline pilot, prolific internationally-published author, national broadcaster, and renowned professional speaker, John’s leadership is propelled by a deep commitment. As a native Texan, John grew up in Dallas, where he earned his bachelor's degree and a Juris Doctor degree from SMU, and is still a licensed Texas attorney. Named Distinguished Alumnus of SMU for 2002, and distinguished Alumnus for Public Service of the SMU Dedman School of Law in 2010, he is also a decorated Air Force pilot veteran of Vietnam and Operations Desert Storm/Desert Shield, and a Lieutenant Colonel in the USAF Reserve, well-known for his pioneering development of Air Force human factors flight safety education, and one of the civilian pioneers of Crew Resource Management (CRM). John has piloted a wide variety of jet aircraft, including most of Boeing's line and the Air Force C-141, and has logged more than 13,900 hours of flight time since earning his first pilot license in 1965; he is still a current pilot. He was a flight officer for Braniff International Airlines and a Boeing 737 Captain for Alaska Airlines, and is an internationally recognized air safety advocate, best known to North American television audiences as Aviation Analyst for ABC World News and Aviation Editor for Good Morning America. Before joining ABC, John logged countless appearances on national shows such as Larry King Live, PBS Hour with Jim Lehrer, Oprah, NPR, Nova, the Today Show, and many others. He is also the nationally-known author of 20 major books, including the acclaimed Why Hospitals Should Fly (2009), and, with co-author Kathleen Bartholomew, Charting the Course (2012). He has also written five non-fiction and 13 international fiction bestsellers. Pandora's Clock and Medusa's Child both aired as major, successful two-part mini-series on television. Why Hospitals Should Fly won the prestigious "Book of the Year" award for 2009 from the American College of Healthcare Executives. John J. Nance has become one of America’s most dynamic and effective professional speakers, presenting riveting, pivotal programs on success and safety in human organizations to a wide variety of audiences, including business corporations and healthcare professionals. He and fellow author Kathleen Bartholomew (Charting the Course and Ending Nurse-to-Nurse Hostility: Why Nurses Eat their Young and Each Other) are highly sought-after for their watershed presentations to boards, senior leaders, physicians, nurses, and staff on quality and patient safety. He is a pioneering and well-known advocate of using the lessons from the recent revolution in aviation safety to equally revolutionize the patient safety performance of hospitals, doctors, nurses, and all of healthcare. Hide bio |
|
See video clip Close Video Clip |
|
|
Kathleen Bartholomew, RN, MN Read bio... Before turning to healthcare as a career in 1994, Kathleen Bartholomew held positions in marketing, business, communications, and teaching. It was these experiences that allowed her to look at the culture of healthcare from a unique perspective and speak poignantly to the issues affecting providers and the challenges facing organizations today. Kathleen Bartholomew, has been a national speaker for the past 12 years. As the manager of a large surgical unit in Seattle, Kathleen quickly recognized that creating a culture where staff felt a sense of belonging was critical to retention. During her tenure as manager, staff, physician, and patient satisfaction reached the top 10% as she implemented her down-to earth strategies. Despite the nursing shortage, Kathleen could always depend on a waiting list of nurses for both units. Kathleen's bachelor's degree is in Liberal Arts with a strong emphasis on Sociology. This background laid the foundation for her to correctly identify the norms and particular to healthcare specifically physician-nurse relationships and nurse-to-nurse hostility. For her master's thesis she authored Speak Your Truth: Proven Strategies for Effective Nurse-Physician Communication, which is the only book to date which addresses physician-nurse issues. In December 2005, Kathleen resigned her position as manager in order to write a second book on horizontal violence in nursing. The expression "why nurses eat their young" has existed for many years in the nursing profession (and has troubled many in the profession). In her book, Ending Nurse to Nurse Hostility (2006), Kathleen offers the first comprehensive and compassionate look at the etiology, impact, and solutions to horizontal violence. Kathleen won the best media depiction of nursing for her op editorial in the Seattle Post-Intelligencer, and in 2010 she was nominated by Health Leaders Media as one of the top 20 people changing healthcare in America. Kathleen's passion for creating healthy work environments is infectious. She is an expert on hospital culture and speaks internationally to hospital boards, the military, leadership, and staff about safety, communication, cultural change, and power. With her husband, John J. Nance, she co-authored Charting the Course: Launching Patient-Centric Healthcare in 2012, which is the sequel to Why Hospitals Should Fly (2008). From the bedside to the boardroom, Kathleen applies research to practice with humor and an ethical call to excellence that ignites and inspires health caregivers and leaders to unprecedented levels of excellence. Hide bio
|
|
|
Susan E. Sheridan, MIM, MBA Read bio... Susan Sheridan, MBA, MIM, is the Deputy Director of Patient Engagement at the Patient-Centered Outcomes Research Institute. She is responsible for creating networks and engaging patients across the nation to provide broad-based input on the development and execution of PCORI’s research. Sheridan became involved in patient safety after her family experienced two serious medical system failures. Her husband, Pat, died in 2002 after his diagnosis of spinal cancer failed to be communicated. Their son, Cal, suffered brain damage called kernicterus five days after his birth in 1995 when his neonatal jaundice was untreated. Sheridan is Co-Founder and a Past President of Parents of Infants and Children with Kernicterus, which works in partnership with private and public health agencies to eradicate kernicterus. In 2003, she co-founded Consumers Advancing Patient Safety (CAPS), a nonprofit organization that seeks a safe, compassionate and just health care system through proactive partnership between consumers and providers of care. Sheridan served at President of CAPS from 2003-2010. From 2004-2011, she led the World Health Organization’s Patients for Patient Safety initiative, which embraces the collective wisdom of the patient, patient empowerment and patient-centered care. Sheridan received her bachelor’s degree from Albion College, and a Masters of International Management and Masters of Business Administration from the Thunderbird School of Global Management. Hide bio |
|
See video clip Close Video Clip |
|
|
Terry Wheat, RN, MPH Read bio... Terry Wheat, RN, MPH, serves as the Director of Patient Care Services & Chief Nursing Officer at Shriners Hospital for Children – Chicago. Under her leadership, the hospital received the 2011 and 2013 Outstanding Nursing Quality Award for pediatric hospital from the American Nurses Association. Mrs. Wheat is on the board of directors for Sinai Health Systems, which includes Mt. Sinai Hospital, Holy Cross Hospital, and Schwab Rehabilitation Hospital. She serves as the chair of the quality & safety committee. Mrs. Wheat has served on the Illinois Emergency Management Service advisory board for seven years representing pediatric rehabilitation. The Governor of Illinois and the Illinois Department of Public Health recently recognized her for dedication and service on the EMSC advisory board.
Mrs. Wheat is an alumna of the University of Illinois, where she obtained both a bachelor's in nursing and a master's in public health in health policy administration. She currently serves as adjunct faculty at the University of St. Francis and the University of Illinois College of Nursing. Hide bio |
|
Global Patient Safety Teams There are numerous opportunities to prevent healthcare accidents. Health Information Technology is an area of great concern to global healthcare leaders. H.I.T offers tremendous potential benefits, however it can introduce risk. The following article addresses the opportunities and the needs for careful adoption of such technologies. The article also addresses a global plan and initiatives that address such risks. Collaborators, please click here to reach training programs. |
CareUniversity Program CareUniversity is a state of the art learning management system coupled to content generation systems that rely on predictive analytics to produce continuing education for caregivers and consumers. The global commitments of CareUniversity include alliances with a number of global organizations including the Conrad Foundation where children are given an opportunity to compete in the development of innovations in health and patient safety. The continuing education content produced with Discovery Channel documentaries are delivered through CareUniversity. |
|
|
|
|
INTRODUCTION
"Trust but verify" is a Russian phrase made famous by President Ronald Reagan during his nuclear arms negotiations with his counterpart Mikhail Gorbachev, who was reported to have said of the President's use of the phrase, "You repeat that at every meeting." [1] Trust but Verify
In 2011, the Institute of Medicine (IOM) released a report on Health Information Technology (HIT) and Patient Safety that clearly articulated the significant risks to patients, provided useful conceptual models, and made recommendations including verification of HIT performance; it also cited the use of existing methods such the Texas Medical Institute of Technology electronic health record computer prescriber order entry (TMIT EHR-CPOE) flight simulator. [2],[3],[4] Late in 2012, the Office of the National Coordinator for Health Information Technology (ONC) of the Dept. of Health and Human Services issued an action plan for public comment acknowledging the IOM report and included recommendations that would "leverage existing federal agency authorities and private sector safety programs to increase knowledge about health IT safety among health care professionals and improve how HIT makes care safer". [5] This article has been posted by TMIT with permission from the Journal of Patient Safety. Download Full Article
|
|
Prior Global Programs
In collaboration with TMIT found at www.safetyleaders.org, we have produced a number of global webinars and programs that may be viewed below.
A Healthcare Cybercrime Classification and Research Report has been produced following analysis of national polling results of quality and safety leaders regarding their interest in the impact of healthcare cybercrime on the medical identities of patients and healthcare professional identities of caregivers and academic leaders. Click here for the report.
Webinars and training provided to our community of practice in patient and caregiver safety will be posted here. The content will include that specifically developed for consumers in association with CareUniversity, our affiliate content developer.
August 15, 2019
Workplace Violence: A Patient and Caregiver Safety Update

 Workplace violence continues to be a critical Patient Safety AND Caregiver issue. Our industry has 4-5 times the frequency of other sectors. Richard Mereu, Chief Government Relations Officer of Government Relations for the Emergency Nurses Association, will address the key issues in their domain. Chief William Adcox and his colleagues at MD Anderson Cancer Center are global experts in Threat Safety Science that includes workplace violence.
Workplace violence continues to be a critical Patient Safety AND Caregiver issue. Our industry has 4-5 times the frequency of other sectors. Richard Mereu, Chief Government Relations Officer of Government Relations for the Emergency Nurses Association, will address the key issues in their domain. Chief William Adcox and his colleagues at MD Anderson Cancer Center are global experts in Threat Safety Science that includes workplace violence.
July 18, 2019
The Quality Journey: The CEO and CMO View
 Dr. J. Michael Henderson and CEO Kevin Cook will address the quality journey of the Chief Medical Officer at the University of Mississippi Medical Center. Dr. Henderson is the former Chief Quality Officer of the Cleveland Clinic and has a long history of work in performance improvement. Kevin Cook is responsible for the strategic leadership of the UMMC Health System, including University Hospital, Wiser Women and Infants Hospital, Conerly Critical Care Hospital, Children’s of Mississippi, UMMC Holmes County and UMMC Grenada, and all UMMC-owned ambulatory clinics.
Dr. J. Michael Henderson and CEO Kevin Cook will address the quality journey of the Chief Medical Officer at the University of Mississippi Medical Center. Dr. Henderson is the former Chief Quality Officer of the Cleveland Clinic and has a long history of work in performance improvement. Kevin Cook is responsible for the strategic leadership of the UMMC Health System, including University Hospital, Wiser Women and Infants Hospital, Conerly Critical Care Hospital, Children’s of Mississippi, UMMC Holmes County and UMMC Grenada, and all UMMC-owned ambulatory clinics.
June 20, 2019
Mortality Reviews and Patient Safety: A 2019 Update

Dr. Jeanne Huddleston is the global pioneer in the use of mortality reviews to improve patient care. She will provide a 2019 update on what has been learned from the world-wide collaborative program she leads. She comes back to us based on popular demand from our patient safety community of practice and the great reviews of her prior presentations that have highlighted Opportunities for Improvement in issues of omission.
May 16, 2019
Drug Diversion Scenarios & An Update on Patient Suicide

 Kim New, JD, BSN, RN, is back speaking about Drug Diversion scenarios to address the growing problem and in response to her extraordinary reviews and number of requests from our community of practice to have her continue to teach and inspire us.
Kim New, JD, BSN, RN, is back speaking about Drug Diversion scenarios to address the growing problem and in response to her extraordinary reviews and number of requests from our community of practice to have her continue to teach and inspire us.
Vicki King is the Assistant Chief of Police at the MD Anderson Cancer Center and UT Health Science Center, UT Police at Houston. She is one of the pioneers of Threat Safety Science and leads a Threat Management team. She will address the latest issues regarding patient suicide prevention.
April 18, 2019
5 Rights of Pain Care, Opioids and Diversion Update

 Dr. Gladstone McDowell is a global leader in pain management who will provide the latest perspective on how best practices in pain management can impact opioid addiction using the 5 Rights of Pain Care framework model.
Dr. Gladstone McDowell is a global leader in pain management who will provide the latest perspective on how best practices in pain management can impact opioid addiction using the 5 Rights of Pain Care framework model.
Kim New, JD, BSN, RN, will be a reactor and provide a short update on the drug diversion issues. David Marx, JD, the founder of the Just Culture movement, will provide his view of the recent Vanderbilt medical error and indictment of a nurse.
March 21, 2019
Serious Adverse Events and Engaging Your Governance Board
 Tom Van Dawark has been a tremendous contributor to healthcare governance. He has been on community and business boards throughout his business career. He has been both a member of the Virginia Mason Hospital and Healthcare System Board Chair, and participated in work with the CEO which resulted in Virginia Mason being recognized today as a top 100 hospital. He is now working closely with boards and championing leadership, patient safety, and governance best practices.
Tom Van Dawark has been a tremendous contributor to healthcare governance. He has been on community and business boards throughout his business career. He has been both a member of the Virginia Mason Hospital and Healthcare System Board Chair, and participated in work with the CEO which resulted in Virginia Mason being recognized today as a top 100 hospital. He is now working closely with boards and championing leadership, patient safety, and governance best practices.
February 21, 2019
From Burnout to Esprit de Corps and Safer Care
 Dr. Stephen J. Swensen, a global expert on leadership and professional burnout, will be speaking on this critical topic. For three decades he has served patients at the Mayo Clinic as its Director of Leadership and Organization Development, Director of Quality, and Chairman of Radiology. Dr. Swensen will address the practical aspects of professional burnout and performance improvement by developing Esprit de Corps. He is now a Professor Emeritus and is very focused on helping organizations develop a safer path for their caregivers and patients.
Dr. Stephen J. Swensen, a global expert on leadership and professional burnout, will be speaking on this critical topic. For three decades he has served patients at the Mayo Clinic as its Director of Leadership and Organization Development, Director of Quality, and Chairman of Radiology. Dr. Swensen will address the practical aspects of professional burnout and performance improvement by developing Esprit de Corps. He is now a Professor Emeritus and is very focused on helping organizations develop a safer path for their caregivers and patients.
January 17, 2019
Sepsis: A 2019 Update on Critical Issues
Casey Clements, MD, PhD, is a renowned emergency medicine physician at the Mayo Clinic who has done a terrific job educating our audience in past webinars. He will update us as of 2019 on the state of the art and care of sepsis. This remains to be one of our most sought after topics and Dr. Clements delivers very practical and actionable information every time he speaks.
December 20, 2018
Respectful Management of Serious Adverse Events: A 2018 Update
 Jim Conway has been a tremendous contributor to what we know about how to handle serious adverse events. An IHI Senior Fellow and frequent speaker on the topic over the years, Jim will provide a 2018 update to the challenges to handling serious adverse events. Heather Foster RN, a frontline nurse who has championed the cause of “taking the high road” will provide her perspective and serve as a reactor.
Jim Conway has been a tremendous contributor to what we know about how to handle serious adverse events. An IHI Senior Fellow and frequent speaker on the topic over the years, Jim will provide a 2018 update to the challenges to handling serious adverse events. Heather Foster RN, a frontline nurse who has championed the cause of “taking the high road” will provide her perspective and serve as a reactor.
November 15, 2018
Highlights of the Last Decade and High Impact Issues for 2019 and Beyond
 John Nance, JD, and a group of safety leaders will help us celebrate this our 120th webinar of our high performer series marking our 10th anniversary. We will be addressing what we have learned from the high impact patient safety target areas of the past and how we can drive accountability for the changes we need in 2019 and beyond as we target issues of Threat Safety Science.
John Nance, JD, and a group of safety leaders will help us celebrate this our 120th webinar of our high performer series marking our 10th anniversary. We will be addressing what we have learned from the high impact patient safety target areas of the past and how we can drive accountability for the changes we need in 2019 and beyond as we target issues of Threat Safety Science.
October 18, 2018
Dauntless Leaders in Nursing: Impacting Patient Safety
 Kathleen Bartholomew, RN, MN is an accomplished author in patient safety with breakthrough professional books such as “Ending Nurse-to-Nurse Hostility” and “Charting the Course” (co-written with John Nance). From the bedside to the boardroom she challenges health care leaders to protect patients with research based presentations woven with narratives that resonate strongly with her audiences. She will address key issues in her latest book “The Dauntless Nurse: Communication Confidence Builder” and how they may empower us our patient safety mission.
Kathleen Bartholomew, RN, MN is an accomplished author in patient safety with breakthrough professional books such as “Ending Nurse-to-Nurse Hostility” and “Charting the Course” (co-written with John Nance). From the bedside to the boardroom she challenges health care leaders to protect patients with research based presentations woven with narratives that resonate strongly with her audiences. She will address key issues in her latest book “The Dauntless Nurse: Communication Confidence Builder” and how they may empower us our patient safety mission.
September 20, 2018
Drug Diversion: The 2018 Crisis Update & Our Future
 Kimberly New has been a terrific speaker for us on drug diversion who is back by popular demand. She is a specialist in controlled substance security and DEA regulatory compliance and consults with healthcare facilities across the country. She is an attorney and an RN who will provide a 2018 update on practical and powerful insights to the exploding drug diversion problem. She is widely published and advises a number of leading medical centers. The webinar for this month is an update to the drug diversion crisis following the excellent and informative programs she led January 18th of 2018 and September 21st of 2017.
Kimberly New has been a terrific speaker for us on drug diversion who is back by popular demand. She is a specialist in controlled substance security and DEA regulatory compliance and consults with healthcare facilities across the country. She is an attorney and an RN who will provide a 2018 update on practical and powerful insights to the exploding drug diversion problem. She is widely published and advises a number of leading medical centers. The webinar for this month is an update to the drug diversion crisis following the excellent and informative programs she led January 18th of 2018 and September 21st of 2017.
August 16, 2018
The HR Department – Friend or Foe: Critical Patient & Caregiver Safety Events
 The Human Resources department at many healthcare organizations have evolved from employee advocacy and concierge functions to becoming an employer’s "defense department". In some cases HR has become weaponized against the very employees who trust them. The trend can put patient safety and quality leaders in a position of distrust with frontline staff. Cynthia Shapiro, a former HR leader and bestselling author of Corporate Confidential will be interviewed and react to caregiver patient safety cases and apply the “50 Secrets” of her book to the healthcare environment. We will discuss the positive ways of ensuring your HR department behaves in a proper manner after an adverse event.
The Human Resources department at many healthcare organizations have evolved from employee advocacy and concierge functions to becoming an employer’s "defense department". In some cases HR has become weaponized against the very employees who trust them. The trend can put patient safety and quality leaders in a position of distrust with frontline staff. Cynthia Shapiro, a former HR leader and bestselling author of Corporate Confidential will be interviewed and react to caregiver patient safety cases and apply the “50 Secrets” of her book to the healthcare environment. We will discuss the positive ways of ensuring your HR department behaves in a proper manner after an adverse event.
July 19, 2018
Healthcare Professional Burnout: A Critical Caregiver & Patient Safety Issue
 Professional Burnout is epidemic in Healthcare Professionals. It negatively impacts both caregivers and patients. Dr. Swensen will present an evidence-based and validated strategy to move from Burnout to Esprit de Corps. Esprit is camaraderie, passion, and engagement wrapped in loyalty to the mission…it recreates fulfillment and joy in practice. Esprit is the single most impactful leading indicator (within our control) of patient experience, outcomes and safety, and driver of organizational effectiveness. Our second speaker, Nancy Conrad, the founder of the Conrad Foundation in honor of Pete Conrad, the astronaut and national hero who died the preventable death of a healthcare systems failure. She will announce the 2018 Global Pete Conrad Patient Safety Award winners.
Professional Burnout is epidemic in Healthcare Professionals. It negatively impacts both caregivers and patients. Dr. Swensen will present an evidence-based and validated strategy to move from Burnout to Esprit de Corps. Esprit is camaraderie, passion, and engagement wrapped in loyalty to the mission…it recreates fulfillment and joy in practice. Esprit is the single most impactful leading indicator (within our control) of patient experience, outcomes and safety, and driver of organizational effectiveness. Our second speaker, Nancy Conrad, the founder of the Conrad Foundation in honor of Pete Conrad, the astronaut and national hero who died the preventable death of a healthcare systems failure. She will announce the 2018 Global Pete Conrad Patient Safety Award winners.
June 21, 2018
Workplace Violence: A Critical Patient and Caregiver Safety Issue
 Workplace violence has become a critical Patient Safety AND Caregiver issue. Our industry has 4-5 times the frequency of other sectors. Chief William Adcox and his colleagues at MD Anderson Cancer Center are global experts in Threat Safety Science that includes workplace violence. He shared the virtual podium with leaders from the healthcare community who will frame the problem and address some of the solutions in the pipeline. Rob Kramer, Director of Government Relations for the Emergency Nurses Association, addressed the key issues in their domain.
Workplace violence has become a critical Patient Safety AND Caregiver issue. Our industry has 4-5 times the frequency of other sectors. Chief William Adcox and his colleagues at MD Anderson Cancer Center are global experts in Threat Safety Science that includes workplace violence. He shared the virtual podium with leaders from the healthcare community who will frame the problem and address some of the solutions in the pipeline. Rob Kramer, Director of Government Relations for the Emergency Nurses Association, addressed the key issues in their domain.
May 17, 2018
Drug Shortages: A Critical Patient Safety Issue
 Drug shortages have become a critical patient safety issue and will continue to be a daunting challenge. Dr. Gregory Botz, Professor of Anesthesia and Critical Care at the MD Anderson Cancer Center and adjunct faculty at Stanford University School of Medicine, is a national patient safety champion who will frame the issue for us. Adriana Rivera, PharmD, will present key strategies and tactics to address this problem. She is a Clinical Pharmacy Specialist at MD Anderson and leader in Pharmacy Medication Management & Analytics.
Drug shortages have become a critical patient safety issue and will continue to be a daunting challenge. Dr. Gregory Botz, Professor of Anesthesia and Critical Care at the MD Anderson Cancer Center and adjunct faculty at Stanford University School of Medicine, is a national patient safety champion who will frame the issue for us. Adriana Rivera, PharmD, will present key strategies and tactics to address this problem. She is a Clinical Pharmacy Specialist at MD Anderson and leader in Pharmacy Medication Management & Analytics.
April 19, 2018
End of Life Care: Learning from Mortality Reviews

 The Opportunities for Improvement (OFI’s) are enormous when it comes to end of life issues. Our audience continuously requests more learning from mortality reviews pioneered by the Mayo Clinic and led by Dr. Jeanne Huddleston. Her emphasis along with other speakers from her research collaborative this month will be on Opportunities for Improvement for the end of life care.
The Opportunities for Improvement (OFI’s) are enormous when it comes to end of life issues. Our audience continuously requests more learning from mortality reviews pioneered by the Mayo Clinic and led by Dr. Jeanne Huddleston. Her emphasis along with other speakers from her research collaborative this month will be on Opportunities for Improvement for the end of life care.
Patty Atkins, MS, RN, FACHE, CPPS, who is Vice President of Quality and Patient Safety at Sharp HealthCare, will discuss this important topic with attention to end of life goals in the ED, a nurse-led approach to end of life issues, and the barriers to nurse-led Advanced Illness Management (AIM) programs.
March 15, 2018
Just Culture – High Impact Case Studies
 In prior webinars, David Marx, JD, established the principles of Just Culture, brought voices from frontline leaders to our audience, and will now present case studies that apply the concepts to real-life scenarios. David Marx draws on experience that spans more than two decades of examining laws, regulations, and industry practices to help lawmakers, regulatory authorities, and organizational leaders fulfill their responsibilities to produce safer outcomes. Our speakers and reactors will discuss applying Just Culture in the real world.
In prior webinars, David Marx, JD, established the principles of Just Culture, brought voices from frontline leaders to our audience, and will now present case studies that apply the concepts to real-life scenarios. David Marx draws on experience that spans more than two decades of examining laws, regulations, and industry practices to help lawmakers, regulatory authorities, and organizational leaders fulfill their responsibilities to produce safer outcomes. Our speakers and reactors will discuss applying Just Culture in the real world.
February 15, 2018
Just Culture – Voices from the Frontline
 David Marx, JD, is a true pioneer in the internationally recognized safety practice of Just Culture. He spoke to our audience in December of 2017 and when we surveyed them, we received an extraordinary response requesting more speakers addressing implementation at the frontline. Our webinar this month fulfills that desire with frontline leaders who will talk about the practical issues of adoption. David Marx draws on experience that spans more than two decades of examining laws, regulations, and industry practices to help lawmakers, regulatory authorities, and organizational leaders fulfill their responsibilities to produce safer outcomes. His colleagues and our reactor panel will explore the drill down issues of adopting and sustaining a truly just culture.
David Marx, JD, is a true pioneer in the internationally recognized safety practice of Just Culture. He spoke to our audience in December of 2017 and when we surveyed them, we received an extraordinary response requesting more speakers addressing implementation at the frontline. Our webinar this month fulfills that desire with frontline leaders who will talk about the practical issues of adoption. David Marx draws on experience that spans more than two decades of examining laws, regulations, and industry practices to help lawmakers, regulatory authorities, and organizational leaders fulfill their responsibilities to produce safer outcomes. His colleagues and our reactor panel will explore the drill down issues of adopting and sustaining a truly just culture.
January 18, 2018
Drug Diversion: A Drill Down Approach
 The webinar for this month is a follow up and detailed approach to the exploding drug diversion problem following an excellent and informative program September 21 of 2017 by Kimberly New. She will drill down on tactical detail regarding how an organization needs to deal with this issue.
The webinar for this month is a follow up and detailed approach to the exploding drug diversion problem following an excellent and informative program September 21 of 2017 by Kimberly New. She will drill down on tactical detail regarding how an organization needs to deal with this issue.
Kimberly New is a specialist in controlled substance security and DEA regulatory compliance and consults with healthcare facilities across the country. She is an attorney and an RN who will provide practical and powerful insights to the exploding drug diversion problem. She is widely published and advises a number of leading medical centers.
December 21, 2017
Just Culture in 2017 and Beyond

 David Marx, JD, is a true pioneer in the internationally recognized safety practice of Just Culture. He draws on experience that spans more than two decades of examining laws, regulations, and industry practices to help lawmakers, regulatory authorities, and organizational leaders fulfill their responsibilities to produce safer outcomes. David will bring us up to date on the state of Just Culture in 2017 and the future as it pertains to patient safety leaders.
David Marx, JD, is a true pioneer in the internationally recognized safety practice of Just Culture. He draws on experience that spans more than two decades of examining laws, regulations, and industry practices to help lawmakers, regulatory authorities, and organizational leaders fulfill their responsibilities to produce safer outcomes. David will bring us up to date on the state of Just Culture in 2017 and the future as it pertains to patient safety leaders.
John Nance, an internationally recognized safety expert in healthcare and aviation who is an award winning author, journalist, attorney, and patient safety advocate will be a reactor to David Marx’s presentation. John is the developer of Red Cover Reports, an NTSB-like approach to analyzing patient safety accidents. William Adcox, the Chief Security Officer for MD Anderson Cancer Center who is also the Chief of Police for the UT Health Science Center and a pioneer of Threat Safety Science will also be a reactor.
November 16, 2017
Sepsis and Triage: Maximizing Safety of Incoming Patients

 Our audience continuously requests more on sepsis. Dr. Jeanne Huddleston, our lead speaker this month, will address this topic to complement our prior sepsis webinars. Her emphasis will be on the triage and safety of incoming patients and the safety of patients being transferred out to other centers. She has led the breakthrough mortality review work at the Mayo Clinic that identified both sepsis and triage as two very important Opportunities for Improvement.
Our audience continuously requests more on sepsis. Dr. Jeanne Huddleston, our lead speaker this month, will address this topic to complement our prior sepsis webinars. Her emphasis will be on the triage and safety of incoming patients and the safety of patients being transferred out to other centers. She has led the breakthrough mortality review work at the Mayo Clinic that identified both sepsis and triage as two very important Opportunities for Improvement.
Dr. Greg Botz and Chief Bill Adcox, both of MD Anderson Cancer Center, and Vicki King of the University of Texas Police at Houston, will provide an update on the Med Tac bystander care program that is focused on patient safety during emergencies threatening the lives of previously healthy children, youth, and adults in their workforce years.
September 21, 2017
Drug Diversion and the Opioid Crisis
 The opioid crisis is touching everyone in our caregiver community. Through multiple recent research surveys, we have found our audience has realized that drug diversion is a patient safety crisis and that we need help at the frontline.
The opioid crisis is touching everyone in our caregiver community. Through multiple recent research surveys, we have found our audience has realized that drug diversion is a patient safety crisis and that we need help at the frontline.
Kimberly New is a specialist in controlled substance security and DEA regulatory compliance and consults with healthcare facilities across the country. She is an attorney and an RN who will provide practical and powerful insights to the exploding drug diversion problem. She is widely published and advises a number of leading medical centers.
August 17, 2017
Sepsis: Bringing it All Together Part 3
 This is the third webinar our sepsis series. Sepsis, according to Dr. Jeanne Huddleston our lead speaker this month, is one of the most common “Opportunities for Improvement” and a great area to have impact. Dr. Huddleston is the leading researcher in mortality reviews at the Mayo Clinic. Our national surveys have revealed that opportunities of omission and sepsis in particular have been identified as a major interest area of our research test bed.
This is the third webinar our sepsis series. Sepsis, according to Dr. Jeanne Huddleston our lead speaker this month, is one of the most common “Opportunities for Improvement” and a great area to have impact. Dr. Huddleston is the leading researcher in mortality reviews at the Mayo Clinic. Our national surveys have revealed that opportunities of omission and sepsis in particular have been identified as a major interest area of our research test bed.
Dr. Huddleston will sum up the terrific presentations in Part 1 and Part 2 and tie what we have learned to what has been gleaned from the Mayo Mortality Review process.
July 20, 2017
The Opioid Crisis: New Threats to Caregivers
 Dr. Gladstone McDowell is one of our nation’s leading pain management experts who has practiced as a urologic oncologist, anesthesiologist, and pain management physician. He frequently speaks to caregivers as well as youth on the dangers of pain medicines and our current opioid crisis. He will address the latest life threatening developments from the introduction of Fentanyl additives to street drugs that are now threatening our first responders, emergency caregivers, and our patients.
Dr. Gladstone McDowell is one of our nation’s leading pain management experts who has practiced as a urologic oncologist, anesthesiologist, and pain management physician. He frequently speaks to caregivers as well as youth on the dangers of pain medicines and our current opioid crisis. He will address the latest life threatening developments from the introduction of Fentanyl additives to street drugs that are now threatening our first responders, emergency caregivers, and our patients.
June 15, 2017
Sepsis: Acute Care Part 2

 This is our second webinar in a series on sepsis. Sepsis, according to Dr. Jeanne Huddleston, the leading researcher in mortality reviews at the Mayo Clinic, is one of the most common “Opportunities for Improvement” and a great area to have impact. Our national surveys have revealed that opportunities of omission and sepsis in particular have been identified as a major interest area of our research test bed.
This is our second webinar in a series on sepsis. Sepsis, according to Dr. Jeanne Huddleston, the leading researcher in mortality reviews at the Mayo Clinic, is one of the most common “Opportunities for Improvement” and a great area to have impact. Our national surveys have revealed that opportunities of omission and sepsis in particular have been identified as a major interest area of our research test bed.
Dr. Huddleston will introduce the topic with a review of the new sepsis related knowledge that has been gleaned from the Mayo Mortality Review process. Casey Clements, MD, PhD, is a renowned emergency medicine physician at the Mayo Clinic who will build on our prior webinar in this second installment on the state of the art care of sepsis.
May 18, 2017
Sepsis: The Basics Part 2

 Sepsis, according to Dr. Jeanne Huddleston, the leading researcher in mortality reviews at the Mayo Clinic, is one of the most common “Opportunities for Improvement” and a great area to have impact. Our national surveys have revealed that opportunities of omission and sepsis in particular have been identified as a major interest area of our research test bed.
Sepsis, according to Dr. Jeanne Huddleston, the leading researcher in mortality reviews at the Mayo Clinic, is one of the most common “Opportunities for Improvement” and a great area to have impact. Our national surveys have revealed that opportunities of omission and sepsis in particular have been identified as a major interest area of our research test bed.
Dr. Ryan Arnold is an emergency medicine physician at Christiana Care Health System and is the Director of Research participating in over 60 different research projects, which include several multi-center clinical trials and investigator-initiated studies. He will be the speaker of the first part of a three part series on sepsis and will provide foundational approach to the issue including important definitions and an evidence based introduction to the topic. A reactor panel of patient advocates and experts will react to the presentation.
April 20, 2017
Failure to Rescue: Bedside Patient Rescue – A Great Opportunity

 Failure to Rescue, according to Dr. Jeanne Huddleston, the leading researcher in mortality reviews at the Mayo Clinic, is one of the most common “Opportunities for Improvement” and a great area to have impact. Opportunities of omission have been identified as a major interest area of our research test bed through multiple surveys. She will introduce the topic and lead our discussions.
Failure to Rescue, according to Dr. Jeanne Huddleston, the leading researcher in mortality reviews at the Mayo Clinic, is one of the most common “Opportunities for Improvement” and a great area to have impact. Opportunities of omission have been identified as a major interest area of our research test bed through multiple surveys. She will introduce the topic and lead our discussions.
Dr. Santiago Romero-Brufau of the Mayo Clinic, will present the Bedside Patient Rescue program developed from the information yielded by mortality reviews as a great opportunity for performance improvement.
 Dr. Jeanne Huddleston presents two back to back sessions regarding the breakthrough work she and her colleagues at the Mayo Clinic have that have had enormous impact on improving quality across their system. She shared learnings on their journey of a detailed data analysis and stories of more than sequential 10,000 patient deaths. She shared the lessons learned through the development and evolution of the Mayo Clinic Mortality Review System and the opportunities to address issues of omission.
Dr. Jeanne Huddleston presents two back to back sessions regarding the breakthrough work she and her colleagues at the Mayo Clinic have that have had enormous impact on improving quality across their system. She shared learnings on their journey of a detailed data analysis and stories of more than sequential 10,000 patient deaths. She shared the lessons learned through the development and evolution of the Mayo Clinic Mortality Review System and the opportunities to address issues of omission.
Mayo Mortality Reviews: Next Generation Patient Safety – The presentation will provides a detailed look at how the Mayo Mortality Review System evolved, their findings, and how barriers were overcome to develop it.
Putting Mortality Reviews to Work – The Enormous Payoff! – The presentation provides a detailed outline and roadmap of how mortality reviews have been put to work at the Mayo Clinic and how other systems in Dr. Huddleston’s national collaborative are undertaking their journeys. The impact of the approach was presented using a comprehensive measurement and improvement approach.
February 16, 2017
Mortality Reviews: Great Learning from Our Early Journey
 Patty Atkins, RN, MS, CNS, CPPS, is responsible for Quality, Patient Safety and Lean Six Sigma for Sharp HealthCare, the largest healthcare system in San Diego, CA. She will share the terrific learning her organization has gleaned from mortality reviews, having worked with Dr. Jeanne Huddleston from the Mayo Clinic who are the leaders in this field. Her insights are just what our surveys have told us from frontline safety leaders in our National Research Test Bed.
Patty Atkins, RN, MS, CNS, CPPS, is responsible for Quality, Patient Safety and Lean Six Sigma for Sharp HealthCare, the largest healthcare system in San Diego, CA. She will share the terrific learning her organization has gleaned from mortality reviews, having worked with Dr. Jeanne Huddleston from the Mayo Clinic who are the leaders in this field. Her insights are just what our surveys have told us from frontline safety leaders in our National Research Test Bed.
Dr. Huddleston's work at the Mayo Clinic has generated one of the strongest positive reactions we have ever had in our nearly 100 monthly sequential webinars. The breakthrough work that can have enormous impact on the patient safety of healthcare institutions.
January 19, 2017
Saving Lives Putting Mortality Reviews to Work – It does pay off!
 Dr. Jeanne Huddleston from the Mayo Clinic generated one of the strongest positive reactions we have ever had in our nearly 100 monthly sequential webinars for her work in mortality reviews. She will now show how such information can be used to save lives.
Dr. Jeanne Huddleston from the Mayo Clinic generated one of the strongest positive reactions we have ever had in our nearly 100 monthly sequential webinars for her work in mortality reviews. She will now show how such information can be used to save lives.
She and her colleagues at the Mayo Clinic have undertaken breakthrough work that can have enormous impact on the patient safety of healthcare institutions. She will share how the learnings on their journey to analyze the stories of all patient deaths are being converted into results. The information Dr. Huddleston shares helps us understand areas of critical importance that will compliment what we do in prevention of adverse events. Following her presentation, a reactor panel will discuss how the insights can be applied to frontline care
December 15, 2016
The Opioid Crisis: An Update for Safety Leaders
 The opioid crisis in America is breathtaking and demands our attention. Dr. Gladstone McDowell is a global leader in pain management who is the Medical Director of Integrated Pain Solutions. He is a trained specialist in Urology, Urologic Oncology, Anesthesiology, Pain Management, and Patient Safety. Dr. McDowell will address the current opioid crisis and updated numbers just reported by the DEA. He will address the issue of gateway drugs and how our healthcare staff, patients, and families are at risk. We will discuss the latest in drug diversion and what safety leaders need to know and watch for in 2017.
The opioid crisis in America is breathtaking and demands our attention. Dr. Gladstone McDowell is a global leader in pain management who is the Medical Director of Integrated Pain Solutions. He is a trained specialist in Urology, Urologic Oncology, Anesthesiology, Pain Management, and Patient Safety. Dr. McDowell will address the current opioid crisis and updated numbers just reported by the DEA. He will address the issue of gateway drugs and how our healthcare staff, patients, and families are at risk. We will discuss the latest in drug diversion and what safety leaders need to know and watch for in 2017.
November 17, 2016
A Safety Leaders Update: Is H.I.T. Evidence Based?
 Ross Koppel, PhD, Adjunct Professor of Sociology, University of Pennsylvania in Philadelphia, has provided tremendous insight to our TMIT audience in the area of E.H.R. patient safety in multiple webinars. He is a leading scholar of healthcare IT, and of the interactions of people, computers, and workplaces. His articles in JAMA, JAMIA, Annals of Internal Medicine, NEJM, Health Affairs, Journal of Patient Safety, the Journal of Clinical Care, Journal of Managed Care, Chest, and AHRQ-M&Ms, et cetera, are considered seminal works.
Ross Koppel, PhD, Adjunct Professor of Sociology, University of Pennsylvania in Philadelphia, has provided tremendous insight to our TMIT audience in the area of E.H.R. patient safety in multiple webinars. He is a leading scholar of healthcare IT, and of the interactions of people, computers, and workplaces. His articles in JAMA, JAMIA, Annals of Internal Medicine, NEJM, Health Affairs, Journal of Patient Safety, the Journal of Clinical Care, Journal of Managed Care, Chest, and AHRQ-M&Ms, et cetera, are considered seminal works.
Dr. Koppel will address a great question: Is Health Information Technology evidence based and what do we need to know?
October 20, 2016
Learning from Collaboration on Mortality Reviews: The Journey

 Dr. Huddleston and her colleagues at the Mayo Clinic have undertaken breakthrough work that can have enormous impact on the patient safety of healthcare institutions. In our July and August webinars, she shared the lessons learned through the development and evolution of the Mayo Clinic Mortality Review System, and will be our introduction speaker for our webinar this month.
Dr. Huddleston and her colleagues at the Mayo Clinic have undertaken breakthrough work that can have enormous impact on the patient safety of healthcare institutions. In our July and August webinars, she shared the lessons learned through the development and evolution of the Mayo Clinic Mortality Review System, and will be our introduction speaker for our webinar this month.
Our audience was polled and asked if they wanted to hear from groups at the front line who have learned from the Mayo Clinic work and are actively studying and collaborating on mortality reviews. Hanan Foley, MSN, RN, CPHQ, the Director of Quality and Safety at MedStar Georgetown University Hospital, will share their experience on the journey.
September 15, 2016
Harmonizing Healthcare Emergency Codes

 Leaders who have successfully harmonized their emergency codes will speak on lessons learned from this vital issue. With the frequency and severity of active shooter events, healthcare facility terrorism, and natural disasters striking healthcare institutions, coordination of the communication of emergency codes is critical. The discussion of the "how to" harmonize emergency codes and implementing plain language and simple text principles to improve effectiveness will be discussed. Stories illustrating how confusion regarding codes can lead to preventable deaths will be shared.
Leaders who have successfully harmonized their emergency codes will speak on lessons learned from this vital issue. With the frequency and severity of active shooter events, healthcare facility terrorism, and natural disasters striking healthcare institutions, coordination of the communication of emergency codes is critical. The discussion of the "how to" harmonize emergency codes and implementing plain language and simple text principles to improve effectiveness will be discussed. Stories illustrating how confusion regarding codes can lead to preventable deaths will be shared.
Dr. Bill Scharf and his colleagues at OSF have successfully accomplished harmonization of emergency codes across their health system and will share their experience. James Mitchell and Aaron Freedkin of Texas Children's Hospital will describe their journey to harmonizing their emergency codes and moving to plain language for the world's largest children's hospital.
In our reactor panel, Chief Bill Adcox, Inspector Vickie King, and Dr. Greg Botz of MD Anderson Cancer Center will discuss the importance of standardization at major medical centers where multiple institutions share common sky walkways and common areas as well as have caregivers and staff who rotate through multiple areas where differing emergency codes are used. Jennifer Dingman will discuss the perspectives of the patient and the family.
August 18, 2016
Learn from Mortality Review AND the Living: Part 2 – A Deeper Dive
 In response to the overwhelmingly positive evaluations of our webinar last month addressing Learning from Mortality Reviews, we have asked Dr. Jeanne Huddleston to take a deeper dive into what can be learned from mortality reviews and how participants can start a program and learn from others. Following her presentation, a reactor panel will discuss the new information building on our July webinar shared by Dr. Huddleston.
In response to the overwhelmingly positive evaluations of our webinar last month addressing Learning from Mortality Reviews, we have asked Dr. Jeanne Huddleston to take a deeper dive into what can be learned from mortality reviews and how participants can start a program and learn from others. Following her presentation, a reactor panel will discuss the new information building on our July webinar shared by Dr. Huddleston.
July 21, 2016
Learn from Mortality Review AND the Living: Next Generation Safety Learning System
Dr. Jeanne Huddleston and her colleagues at the Mayo Clinic have undertaken breakthrough work that can have enormous impact on the patient safety of healthcare institutions. She will share learnings on their journey to analyze the stories of all patient deaths. She will share the lessons learned through the development and evolution of the Mayo Clinic Mortality Review System.
Patient safety events are increasingly recognized as the 3rd leading cause of death including the typical adverse events we count and measure in patient safety. These existing measurement systems do not identify actionable opportunities for improvement nor provide obvious direction for next steps. The information Dr. Huddleston will share will help us understand areas of critical importance that will compliment what we do in prevention of adverse events. Following her presentation, a reactor panel will discuss the new information shared by Dr. Huddleston.
June 16, 2016
New Oral Anticoagulants: New Patient Safety Challenges
Dr. Alan Jacobson is a pioneer and leader in the field of anticoagulation management, having implemented innovative strategies within the VA system to improve anticoagulation management and dramatically reducing risk with out-of-range INR and complications associated with anticoagulation therapy.
Dr. Jacobson addressed the challenges associated with the new therapeutic drugs, which require less monitoring, but bring new risks. There are new lessons being learned that can help keep patients safer when these innovative new medications are being used.
The May webinar addressed other leading causes of death of students K-12, colleges, and young employees. The topics include practical issues addressing Opioid Overdose, Anaphylaxis, Cardiac Arrest, Choking, On-site Transportation accidents, Bullying and Abuse of Power that can lead to workplace and school violence, active shooter events, and the value of a Rapid Response Team approach in schools and institutions. Our audience response to the May webinar covering Opioid related adverse events was terrific and led us to take a deep dive on the leading causes of death of young people – students at schools, colleges, and on the job.
We were proud to have Dr. Greg Botz, a national Intensive Care and patient safety leader, address the High Impact Care Hazards facing schools, colleges, and healthcare institutions. He will address the critical knowledge, lifeline behaviors or competencies that  m
m ust be learned, and how assessment of such competencies may be undertaken. We introduced a new Medical-Tactical Certificate program that students can help lead in their school, college, or medical school.
ust be learned, and how assessment of such competencies may be undertaken. We introduced a new Medical-Tactical Certificate program that students can help lead in their school, college, or medical school.
Dr. Toff Peabody, a leading Emergency Medicine physician, updated us on the Dream Team concept successfully used in graduate training programs to combat burn out and introduce a new program being launched for Pre-med students. Students from leading Texas universities will reacted to the discussions as well as leading patient advocates.
April 28, 2016
The Opioid Patient Safety Crisis: Actions and Reactions
 Opioid related adverse events have become a critical patient safety issue as evidenced by actions taken last month by the FDA (see link: http://www.fda.gov/NewsEvents/Newsroom/FactSheets/ucm484714.htm) and CDC (see link: http://www.cdc.gov/drugoverdose/prescribing/guideline.html).
Opioid related adverse events have become a critical patient safety issue as evidenced by actions taken last month by the FDA (see link: http://www.fda.gov/NewsEvents/Newsroom/FactSheets/ucm484714.htm) and CDC (see link: http://www.cdc.gov/drugoverdose/prescribing/guideline.html).
We were proud to have Dr. Gladstone McDowell as our speaker; Dr. McDowell spoke extensively on the topic of pain management and the use and misuse of opioid medications. He discussed the latest patient safety developments and current strategies to optimize opioid use in the context of the "5 Rights of Pain Care®." After his presentation, Dr. McDowell was joined by members of a reactor panel who discussed the key takeaways with our experts, and responded to questions from our webinar participants.
January 21, 2016
Health Information Technology Safety Community of Practice
 TMIT was delighted to have Ross Koppel, PhD, Adjunct Professor of Sociology, University of Pennsylvania in Philadelphia. His presentation "From MU to MUch less? What is CMS telling us?" We were also delighted to have Christopher Peabody, MD, MPH, Assistant Clinical Professor of the Department of Emergency Medicine, University of California in San Francisco, lead the launch of our Community of Practice. He presented "Health IT: Front-line Problems and Solutions." John Nance, a world-class speaker, joined these presenters covering "HIT Accidents and Cybercrime Issues," along with Dan Ford, one of our nation's leading patient advocates, who gave his talk on "Reflections on Visioning E.H.R. Vendor Transition and Including Patient Advocates."
TMIT was delighted to have Ross Koppel, PhD, Adjunct Professor of Sociology, University of Pennsylvania in Philadelphia. His presentation "From MU to MUch less? What is CMS telling us?" We were also delighted to have Christopher Peabody, MD, MPH, Assistant Clinical Professor of the Department of Emergency Medicine, University of California in San Francisco, lead the launch of our Community of Practice. He presented "Health IT: Front-line Problems and Solutions." John Nance, a world-class speaker, joined these presenters covering "HIT Accidents and Cybercrime Issues," along with Dan Ford, one of our nation's leading patient advocates, who gave his talk on "Reflections on Visioning E.H.R. Vendor Transition and Including Patient Advocates."
|
Prior Global Summits |
||||||||||||
|
|
|
|
|
| Charles Denham, MD: TMIT; Harvard ALI David Hunt, MD, FACS: U.S. Department of Health & Human Services Dana Rohrabacher, MA: U.S. House of Representatives, R-CA Dennis Wagner, MPA: Centers for Medicare & Medicaid Services Chesley B. (Sully) Sullenberger III: Pilot, U.S. Airways (Retired) John Nance, JD: Best-selling Author and Pilot James Bagian, MD, PE: University of Michigan David W. Bates, MD, MSc: Brigham and Women's Hospital David Classen, MD, MS: University of Utah Paul McGann, MD: Centers for Medicare & Medicaid Services Samantha M. Chao, MPH: Institute of Medicine Leah Binder, MA, MGA: The Leapfrog Group Perry Bechtle, DO: Mayo Clinic, Jacksonville, FL William Munier, MD, MBA: U.S. Department of Health & Human Services Arjun Srinivasan, MD: Centers for Disease Control and Prevention Jean D. Moody-Williams, RN, MPP: Centers for Medicare & Medicaid Services Farzad Mostashari, MD, ScM: U.S. Department of Health & Human Services |
Stephen Swensen, MD, MMM, FACR: Mayo Clinic College of Medicine J. Michael Henderson, MD: Cleveland Clinic Health System Mike Williams, MD, MBA: Hill Country Memorial Hospital Robert Chapman, MBA: Barry-Wehmiller Companies, Inc. Regina Holliday: Patient Rights Arts Advocate Trisha Torrey: Patient Advocate Lygeia Ricciardi, EdM: U.S. Dept. of Health & Human Services Mary Foley, RN, PhD: University of California Nancy Conrad: Conrad Foundation Sharon Rossmark, MBA: Zayos Global Ventures, LLC David Parda, MD, FACP: Allegheny General Hospital Ellen Canepa Brzytwa, RN, MSN, MPH: Ellen Brzytwa and Associates Gladstone C. McDowell, II, MD: Integrated Pain Solutions; TMIT Franck Guilloteau: Texas Medical Institute of Technology (TMIT) Thomas Zeltner, MD: Fondation Science et Cité, Switzerland Edward Kelley, PhD: World Health Organization, Switzerland |
Collaboration Best Practices |
|
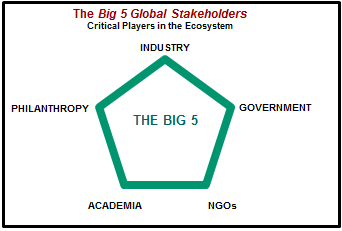 |
|
|
The critical stakeholders who must weigh in on rapid response teams for crises in healthcare are Industry, Government, Non-government Organizations, Academia, and Philanthropy. Often they are competitors and have numerous conflicts of interest, however they must work together to drive life-saving innovations. |
A major area of focus of our group will be the issue of supplier funded research with providers and academia. We will take a systematic approach to frameworks that provide a "safe harbor" for supplier funded research and development. The Forum has ongoing global research and development activities that address turning barriers into accelerators at the supplier-provider interface and at the provider-purchaser interface. |
 |
|
|
The interface areas between trading partners along the healthcare supply chain are major barriers to patient safety innovations, however when issues such as conflicts of interest are dealt with using best practices, patient safety can be dramatically improved. |
Members of the GPSF collaborative initiatives addressing barriers and accelerators may access these programs, however they are password protected. Please click here to access. |
Governance Leaders Programs: |
| Governance, administrative, and medical leaders have the ability to make transformational impact on patient safety and systems performance. The GPSF is focused on accelerating the adoption of high performance patient safety solutions that leverage engaged leaders, practices that deliver predictable outcomes, and the technologies that enable them. The GPSF is leveraging opportunities at the intersection of these three spheres, such as the Governance Quality Training Program called CareBoards, distributed through CareUniversity. The documentary Surfing the Healthcare Tsunami: Bring Your Best Board is a film targeting governance leaders as untapped power. Click here to view the full length film for free. The Pete Conrad Patient Safety Excellence Award was created in honor of the astronaut, Pete Conrad, who died the preventable death of a systems failure. The award recognizes organizations and individuals that have made significant impact in patient safety through their work and enduring commitments to improving the quality and safety of healthcare for everyone. Click here for more about this award. |
 |
|
|
John J. Nance, JD One of the key thought leaders to emerge in American healthcare in the past decade, John J. Nance brings a rich and varied professional background to the task of helping doctors... Read bio... One of the key thought leaders to emerge in American healthcare in the past decade, John J. Nance brings a rich and varied professional background to the task of helping doctors, administrators, boards, and front-line staff alike survive and prosper during the most profoundly challenging upheaval in the history of modern medicine. Having helped pioneer the renaissance in patient safety as one of the founders of the National Patient Safety Foundation in 1997, his efforts (and healthcare publications) are dedicated to reforming American healthcare from a reactive cottage industry to an effective and safe system of prevention and wellness. A lawyer, Air Force and airline pilot, prolific internationally-published author, national broadcaster, and renowned professional speaker, John's leadership is propelled by a deep commitment.
As a native Texan, John grew up in Dallas where he earned his bachelor's degree and a Juris Doctor degree from SMU, and is still a licensed Texas attorney. Named Distinguished Alumnus of SMU for 2002, and distinguished Alumnus for Public Service of the SMU Dedman School of Law in 2010, he is also a decorated Air Force pilot veteran of Vietnam and Operations Desert Storm/Desert Shield, and a Lieutenant Colonel in the USAF Reserve, well-known for his pioneering development of Air Force human factors flight safety education, and one of the civilian pioneers of Crew Resource Management (CRM). John has piloted a wide variety of jet aircraft, including most of Boeing's line and the Air Force C-141, and has logged more than 13,900 hours of flight time since earning his first pilot license in 1965; he is still a current pilot. He was a flight officer for Braniff International Airlines and a Boeing 737 Captain for Alaska Airlines, and is an internationally recognized air safety advocate, best known to North American television audiences as Aviation Analyst for ABC World News and Aviation Editor for Good Morning America. Before joining ABC, John logged countless appearances on national shows such as Larry King Live, PBS Hour with Jim Lehrer, Oprah, NPR, Nova, the Today Show, and many others. He is also the nationally-known author of 20 major books, including the acclaimed Why Hospitals Should Fly (2009), and, with co-author Kathleen Bartholomew, Charting the Course (2012). He has also written five non-fiction and 13 international fiction bestsellers. Pandora's Clock and Medusa's Child both aired as major, successful two-part mini-series on television. Why Hospitals Should Fly won the prestigious "Book of the Year" award for 2009 from the American College of Healthcare Executives. John J. Nance has become one of America's most dynamic and effective professional speakers, presenting riveting, pivotal programs on success and safety in human organizations to a wide variety of audiences, including business corporations and healthcare professionals. He and fellow author Kathleen Bartholomew (Charting the Course and Ending Nurse-to-Nurse Hostility: Why Nurses Eat their Young and Each Other) are highly sought-after for their watershed presentations to boards, senior leaders, physicians, nurses, and staff on quality and patient safety. He is a pioneering and well-known advocate of using the lessons from the recent revolution in aviation safety to equally revolutionize the patient safety performance of hospitals, doctors, nurses, and all of healthcare. Hide bio |
|
Sharon Rossmark, MBA Sharon Rossmark is System Vice Chair for The Sinai Health System in Chicago, Illinois. She also serves as board chair for Patient Safety and sits on the Public Policy, Compensation, and Finance/Audit Committees. Read bio... Sharon Rossmark is System Vice Chair for The Sinai Health System in Chicago, Illinois. She also serves as board chair for Patient Safety and sits on the Public Policy, Compensation, and Finance/Audit Committees. As a board member she has participated in legislative advocacy meetings with Congressional leaders on Capitol Hill and at the White House. The Sinai Health System entities include Mount Sinai Hospital; Sinai Children's Hospital; Schwab Rehabilitation Hospital; Sinai Medical Group; Sinai Community Group; and Sinai Urban Health Institute.
Ms. Rossmark also currently serves as a hospital trustee representative on the American Hospital Association's Midwest Regional Policy Board, and has been appointed to serve as a governance expert on the editorial advisory board of the Journal of Patient Safety, a global peer-reviewed publication. Ms. Rossmark's board experience also includes board appointments to the National Children's Center in Washington, DC, and the College of Business Advisory Board at Illinois State University. Previously, she served on The Allstate Foundation Board and on the Board of Trustees for Oakton Community College. She is a member of the National Association of Corporate Directors and the American Hospital Association Trustee Leadership Network. She also has been a frequent panel facilitator and panelist. Ms. Rossmark's business experience includes currently serving as President and CEO of Zayos Global Ventures, LLC, a worldwide liquidation and distribution business providing integrated e-commerce consulting solutions. Previously, she worked for 30 years in the financial services and insurance industry including an appointment as an executive for a Fortune 100 company. To honor her parents and her father's WWII D-Day service, Ms. Rossmark has established an endowed scholarship to support U.S. military soldiers and veterans majoring in business at Illinois State University. Ms. Rossmark earned her MBA from the University of Illinois – Chicago, and an undergraduate degree from Illinois State University. Hide bio |
|
|
Ellen Canepa Brzytwa, RN, MSN, MPH Ellen Canepa Brzytwa, RN, MSN, MPH, is a consultant and civic activist in the Greater Cleveland area. She is the principal of Ellen Brzytwa and Associates, a healthcare consulting group, and consults on healthcare research; Read bio... the design of integrated delivery systems of healthcare; institutional advancement; board governance issues; and the nursing profession. Ms. Brzytwa is a trustee for Lakewood Hospital, a member hospital of the Cleveland Clinic Health System. In 2011, Ms. Brzytwa served on an enterprise-wide Quality Task Force of select members of all the Cleveland Clinic hospitals' governing boards to design a pioneering governance approach to establish system-wide quality goals; review global quality data and high-level hospital data; and monitor quality and safety performance in coordination with all enterprise governing boards and their quality committees. In 2012 this work will be done by the Cleveland Clinic Safety, Quality and Patient Experience Committee, with Ms. Brzytwa as a community trustee member. Hide bio |
David S. Parda, MD, FACP David S. Parda, MD, FACP, is System Chair of the Department of Radiation Oncology, Allegheny General Hospital (AGH) and Read bio... West Penn Allegheny Health System (WPAHS) Radiation Oncology Network. He has developed eight primary programs in radiation oncology (clinical program, technical program, clinical research program, IT program, residency training/education program, industry collaboration program, translational/correlative science program, community outreach program) to integrate a network of 11 radiation oncology clinics in Western Pennsylvania and Eastern Ohio with advanced technologies and data collection processes to optimize standard and advancing patient care. This has resulted in one of the nation's most expert and comprehensive radiation oncology centers at AGH and throughout WPAHS Radiation Oncology Network, which is recognized regionally, nationally, and internationally as a leading academic radiation oncology program. Dr. Parda received his Bachelor of Arts degree with honors in molecular biology and psychology from Vanderbilt University, and his medical degree from the University of South Florida College of Medicine. He completed a residency in internal medicine at the Cleveland Clinic Foundation and a residency in radiation oncology at Georgetown University, and is board certified in both internal medicine and radiation oncology. Through special training at the National Cancer Institute (NCI) Laboratory of Cellular and Molecular Biology, Georgetown University's Lombardi Cancer Center, and Memorial Sloan-Kettering Cancer Center, Dr. Parda has acquired noted expertise in the multidisciplinary treatment of cancer. His clinical and research interests include breast cancer; colorectal cancer; head and neck cancer, including eye and orbit; Intensity-Modulated Radiation Therapy (IMRT); Image-Guided Radiation Therapy (IGRT); Adaptive Radiation Therapy (ART); functional and 4-D data incorporation into radiation treatment planning; oncology information systems/electronic medical record integration processes; clinical trials and correlative/translational science research; medical education; quality assurance/peer review; and brachytherapy. Dr. Parda has held appointments as an assistant professor of radiation oncology at Georgetown University, MCP Hahnemann University School of Medicine, and the University of Pittsburgh School of Medicine, and as an associate professor of radiation oncology at Drexel University College of Medicine. He is currently serving as Professor at Temple University School of Medicine. He served as the Radiation Oncology Residency Program Director at Allegheny General Hospital from 2000 to 2009, and currently maintains involvement with educational programs as Associate Residency Program Director. He is a member of the American College of Radiology and Radiation Oncology; the American Medical Association; the American Society for Radiation Oncology; and the Society of Chairs of Academic Radiation Oncology Programs. Dr. Parda serves on the American Society for Radiation Oncology Best Practices Committee with 11 other radiation oncology experts from the United States. Having been selected among 10 leading oncology experts from the U.S., Europe, and Asia, he is also a the physician representative from the U.S. of an International Oncology Experts Group that is mapping the future of radiation oncology, technology, and advanced oncology work-flow over the next several years. He is an Associate Director and Radiation Oncology Protocol Officer for the National Surgical Adjuvant Breast and Bowel Project (NSABP), an NCI-sponsored Phase 3 cancer clinical trials group; Chair of the NCI Central Institutional Review Board (2011-2013); an examiner for the American Board of Radiology Radiation Oncology Resident Oral Board Examination; a board member and president-elect of the Pennsylvania Society of Oncology and Hematology; a past Director-At-Large on the Pennsylvania Board of Directors of the American Cancer Society; Chair of the West Penn Allegheny Health System Institutional Review Board; Chair of the WPAHS Oncology Service Line; Chair of the WPAHS Values Team; and Chair of the WPAHS Physician Compensation and Productivity Committee. Dr. Parda is also a member of the West Penn Allegheny Health System Board of Directors; the Medical Research, Education and Affairs Committee; and the Finance and Operations Committee. Hide bio |
|||
|
Perry S. Bechtle, DO Perry S. Bechtle, DO, is a neuroanesthesiologist at Mayo Clinic in Florida and served as the Division Chairman of Neuroanesthesiology from 1997 to 2010. He also serves as the Patient Safety Officer and quality leader within the Department of Anesthesiology... Read bio... and is a Mayo Quality Fellow and the Medical Director of the Interventional MRI (IMRIS) neurosurgical suite. Prior to joining Mayo Clinic, he was a U.S. Naval flight surgeon for five years, then completed anesthesiology residency training at Mayo Clinic in Florida and a neuroanesthesia fellowship at Mayo Clinic in Rochester, MN. Dr. Bechtle's experience in other high-consequence industries includes being the flight surgeon for the U.S. Navy Flight Demonstration Squadron, the Blue Angels, from 1992 to 1994; work as a subcontractor at NASA Johnson Space Center Medical Operations in Houston and as Safety Coordinator at one of the Space Shuttle East coast alternate landing sites at MCAS Cherry Point, NC; and employment as Space Shuttle launch and recovery physician with the Department of Defense Division for Manned Space Flight at Kennedy Space Center in Florida. He has been a consultant to Medtronic Xomed, primarily assisting with health hazard evaluation and failure mode effects analysis on a variety of products. With a technical background in industrial safety and aviation safety, and a career which still includes daily work in the neurosurgical operating rooms of Mayo Clinic in Florida, Dr. Perry Bechtle brings a balanced, practical perspective to the organizational goal of achieving individual habitual excellence, true teamwork, vertical communication, and safety resilience in both patient safety and worker safety. Hide bio |
Christopher R. Peabody, MD, MPH Dr. Peabody is a practicing Emergency Physician in California and Clinical Instructor at the University of California, San Francisco. He is also the Director of the UCSF Acute Care Innovation Center... Read bio... Sharon Rossmark
an initiative of the UCSF Department of Emergency Medicine, which develops novel ways to deliver Emergency and Acute Care reliably and safely by developing new technology and validating best practices. He has a strong commitment to public service and healthcare delivery to vulnerable populations. Dr. Peabody completed his residency at one of the busiest safety-net hospitals in the country, Los Angeles County Hospital, and was the Chief Resident in Emergency Medicine at the University of Southern California. He attended medical school at the University of California San Francisco, and completed an MPH at Harvard University on a Zuckerman Fellowship. Dr. Peabody's current interests lie in quality improvement and patient safety, especially related to underserved populations. He has extensive experience in emergency care and disaster response internationally, having served in Haiti and China. He is a member of the content leadership development team for CareUniversity and applies his expertise in emergency care, public health, and international healthcare performance improvement to meeting the needs of both consumers and caregivers. Hide bio |
|||
|
Kathleen Bartholomew, RN, MN Before turning to healthcare as a career in 1994, Kathleen Bartholomew held positions in marketing, business, communications, and teaching. It was these experiences that allowed her to look at the culture of healthcare from a unique perspective and speak poignantly to the issues affecting providers and the challenges facing organizations today. Read bio... Kathleen Bartholomew, RN, MN, has been a national speaker for the past 12 years. As the manager of a large surgical unit in Seattle, Kathleen quickly recognized that creating a culture where staff felt a sense of belonging was critical to retention. During her tenure as manager, staff, physician, and patient satisfaction reached the top 10% as she implemented her down-to earth strategies. Despite the nursing shortage, Kathleen could always depend on a waiting list of nurses for both units.
Kathleen's bachelor's degree is in Liberal Arts with a strong emphasis on Sociology. This background laid the foundation for her to correctly identify the norms and particular to healthcare – specifically physician-nurse relationships and nurse-to-nurse hostility. For her master's thesis she authored Speak Your Truth: Proven Strategies for Effective Nurse-Physician Communication, which is the only book to date which addresses physician-nurse issues. In December 2005, Kathleen resigned her position as manager in order to write a second book on horizontal violence in nursing. The expression "why nurses eat their young" has existed for many years in the nursing profession (and has troubled many in the profession). In her book, Ending Nurse to Nurse Hostility (2006), Kathleen offers the first comprehensive and compassionate look at the etiology, impact, and solutions to horizontal violence. Kathleen won the best media depiction of nursing for her op editorial in the Seattle Post-Intelligencer, and in 2010 she was nominated by Health Leaders Media as one of the top 20 people changing healthcare in America. Kathleen's passion for creating healthy work environments is infectious. She is an expert on hospital culture and speaks internationally to hospital boards, the military, leadership, and staff about safety, communication, cultural change, and power. With her husband, John J. Nance, she co-authored Charting the Course: Launching Patient-Centric Healthcare in 2012, which is the sequel to Why Hospitals Should Fly (2008). From the bedside to the boardroom, Kathleen applies research to practice with humor and an ethical call to excellence that ignites and inspires health caregivers and leaders to unprecedented levels of excellence. Hide bio |
Mary E. Foley, RN, PhD Mary E. Foley, RN, PhD, is the Director in the Center for Nursing Research and Innovation at the University of California, San Francisco (UCSF). Read bio... She has worked with the Center as Associate Director since 2004 in partnership with three Bay Area academic medical centers. Mary has worked with the Collaborative Alliance for Nursing Outcomes (CALNOC) since 2004, and in 2009 was appointed Director, Education Services for CALNOC. In that role, Mary has developed an area of expertise in nursing sensitive care measures, with special emphasis on medication safety. Mary was president of the American Nurses Association from 2000-2002. She was employed for 19 years at Saint Francis Memorial Hospital in San Francisco where she worked as a staff nurse, Director of Nursing, and Safety Officer. A registered nurse for more than 35 years, Foley has been active in the healthcare policy arena. She continues to write and lecture about healthcare policy, improving the workplace, and promoting safe care for workers and patients. She completed a six-year term as a member of the National Patient Safety Foundation Board of Directors, and is an advisory member of the Partnership for Patient Safety (p4ps). She is a member of the TMIT Patient and Family Advisory panel. She also continues to work with TDICT as a project consultant with expertise in needle stick injury prevention device evaluation. Foley received her nursing diploma in 1973 from New England Deaconess Hospital School of Nursing; her BSN in 1976 from Boston University School of Nursing in Massachusetts; and her Master's of Science in Nursing Administration and Occupational Health from the University of California in San Francisco in 1994. She completed her doctoral studies at UCSF in the spring of 2010 with an emphasis on policy and occupational health. Hide bio |
|||
|
Jennifer Dingman Jennifer Dingman realized, after her mother's death in 1995 due to errors in medical diagnoses and treatment, that there is little to no help available for patients and their families in similar situations. Read bio... This life-changing experience left her feeling vulnerable, and she decided to dedicate her life to help prevent medical tragedies from happening to others. In 1996, Jennifer founded PULSE of Colorado, now a national organization, as a platform to support patients and their families who had experienced medical errors and other adverse medical outcomes. Within two years, PULSE became a national force when PULSE of New York paved the way for many other state chapters to be born. Additionally, Jennifer became an active member of the National Patient Safety Foundation and served on numerous committees, including the Board of Governors. For more than 15 years, she has volunteered her time to improve the quality of the healthcare system in the U.S. She believes that patient involvement, and promoting an equal partnership between the doctor and the patient, is the most effective way to achieve better quality in the healthcare industry. Jennifer is a TMIT Patient Advocate Team Member. She has co-authored patient safety articles in peer-reviewed medical journals. She is a member of Champion for Patient Safety, and represented the organization at the 2005 Patients for Patient Safety Workshop in London and the 2006 Pan American Health Organization Workshop in San Francisco to discuss patient safety and empowerment. Jennifer also served on the board of directors for a local Colorado-based community health center for six years and currently sits on the local school district's health advisory board. An avid patient advocate, Jennifer Dingman joined the Cautious Patient Foundation as an Advisory Board member. In this position, Jennifer offers input, ideas and expert advice on the Foundation's key issues in order to bring changes to the current healthcare system. Since 2009, Jennifer has served as a faculty member of The Patient Safety Clinical Pharmacy Collaborative, a groundbreaking patient safety initiative that has changed the face of healthcare delivery with measureable positive outcomes for patients. For her tireless efforts, she has won national recognition, including the 2004 Patient Safety Award given by the Colorado Patient Safety Coalition, where Jennifer is a member, and the 2007 Pete Conrad Patient Safety Award. Her invaluable input from a patient's perspective is widely sought by healthcare groups that are addressing patient-safety issues. Jennifer's energy and compassion help both patients and doctors alike. Hide bio |
Becky Martins Becky Martins' advocacy spirit derives from the days when she was driving a family member 150 miles round-trip, three days a week, to dialysis treatments. She spent countless hours at the unit visiting with patients and their families. Read bio... Sharon Rossmark
It was through their stories that she learned of the many challenges faced by patients living with chronic illness. It was by their example that she learned of the resilience of the human spirit to face health and health-related challenges head-on. The unit was her classroom, and her teachers were the patients and families, along with the unit staff who cared for them. The experience became the impetus for her advocacy on behalf of end-stage renal disease patients. In 1996, Becky was the recipient of the Kidney Foundation of Maine Board of Trustees' Service Award for 10 years of service. In 2002, Becky founded Voice4Patients.Com: an initiative to empower patients to be their own health care advocates. The site advocated building partnerships between patients and providers – and provided information and tools to strengthen consumer skills. Becky Martins is a champion of patient- and family-centered care, effective communication in health care, and patient and family involvement: from the board room to examining room. She is a TMIT Patient Advocate Team Member; a Patients for Patient Safety Champion of the World Healthcare Organization's World Alliance of Patient Safety; and a past member of National Patient Safety Foundation's Patient & Family Advisory Councils. She was a contributor to "Opportunities for Patient and Family Involvement" – Chapter Nine of the National Quality Forum's Safe Practices for Better Healthcare – 2009 Update: A Consensus Report. The 121st Maine Legislature presented Ms. Martins with a Special Sentiment for her patient safety advocacy. She is a recipient of the Pete Conrad Patient Safety Excellence Award. Hide bio |
|||
|
Arlene Salamendra Arlene Salamendra is a former Board member and Staff Coordinator of Families Advocating Injury Reduction (FAIR). A number of years ago, she was the subject of a preventable medical error. Since that time, she has devoted a portion of her time to giving support to other patients... Read bio... who have been injured or have lost a loved one, and rectifying the systems errors that lead to preventable medical errors. She is a member of the TMIT Patient Advocate Team. Hide bio |
Dan Ford, MBA, LFACHE Dan Ford developed a deep passion for patient safety as a result of medical errors experienced in Illinois by his first wife, Diane, and the treatment he experienced when he started asking logical and genuine questions. Read bio... The mother of three children (11, 14, and 17 at the time) and age 47, Diane was pursuing her second master’s degree, and suffered a morphine-induced respiratory arrest following a hysterectomy. She has permanent brain damage/short-term memory loss and a poor quality of life, and resides in an independent living facility. Desiring to convert his anger, hurt, and frustration into constructive change – delayed because of a nine-year medical malpractice lawsuit – and using his visibility as a healthcare executive search consultant, Dan became a patient safety advocate in 2002. He has given 90 patient safety presentations to boards of directors, management, and physician leadership of hospitals, systems, other provider organizations, and HRSA. He is a CAPS member and WHO/PAHO champion, and works with TMIT and a group of other patient safety advocates on listening, disclosure, and related initiatives. He has served on a number of other provider patient safety and quality committees nationally and in Arizona, including ISMP, NQF, The Joint Commission, IHI, AzHHA, Catholic Health Partners, and Carondelet Health Network. He helped to plan and facilitate CAPS “Partnering with Provider” workshops at Northwestern Memorial in Chicago, Johns Hopkins in Baltimore, and AzHHA in Phoenix in 2008 and 2009. In 2010, Dan was a co-author, with Bev Johnson and Marie Abraham, of “Collaborating with patients and their families” in the Journal of Healthcare Risk Management, the journal of the American Society for Healthcare Risk Management. The story of serious medical errors experienced by Dan’s wife and the impacts his family has endured is told in a chapter of Dr. Sanjay Kumar’s book, Fatal Care: Survive in the U.S. Health System. Dan authored an article on patient and family involvement in root cause analyses, which appeared in the December 2013 online issue of Dorland Health’s Case in Point. Dan is a retired Vice President with Furst Group, a national healthcare executive search firm headquartered in Rockford, Illinois. His MBA is from the University of Chicago, preceded by a BS from Jamestown University in North Dakota. He was in the Navy from 1964-69, a Naval Aviator in a transport squadron which serviced the fleet in the Pacific during the Vietnam War. Hide bio |
|||
"We will measure our success by how we protect and enrich the lives of families."
| CareUniversity. CareU was developed in response to enormous unmet needs expressed by families and professional caregivers. Not a college or university, it partners with higher education institutions to deliver knowledge that can earn course credit and certificates of completion as well as novel incentives for consumers. High Impact Care Hazards: There are certain conditions that are frequent and severe that can be prevented by new consumers and caregiver behaviors. We call these conditions that can threaten the physical and financial health of everyone "high impact care hazards". |
Lifeline Behaviors: The new behaviors that can protect us, we call "lifeline behaviors". They can be taught online, in groups, and in many new ways such as over mobile phones. CareUniversity connects people to great resources and does not compete with medical, nursing, and pharmacy schools. It compliments their curricula with practical concepts, tools, and resources. Competency Currency: It is critical that the competency of new lifeline behaviors or skills be maintained. So for certain courses and programs, CareU has modeled its program of re-certification of competencies after the aviation industry. |
More than 70% of healthcare decisions are made by women in our communities. More than 90 million Americans are a caregiver of someone else and two thirds of the caregivers are women. This pattern is very similar across the world regardless of the income status and seen in low income, emerging, and industrialized nations. Although much fewer in number as a community force, there are many CareDads who are taking the lead fortheir families health and well-being and there are many coaches and mentors who are also looking out for our nation's children. There are many sons, daughters, and other family members taking care of their parents as well. |
The CareMoms program and training through CareUniversity have been designed to support a grassroots effort to engage our community CFOs – Chief Family Officers – to prevent healthcare accidents in their families. CareMoms can help them rally and support their local hospitals to win the war on healthcare harm and prevent common healthcare accidents in certain very common "High Impact Care Conditions" in acute care, chronic care, and preventive care. |
| CareKids is an initiative of CareUniversity that leverages the enormous innovation talent of the truly first native digital generation. In collaboration with the Conrad Foundation that was established in honor of Pete Conrad, the third man to walk on the moon. Children from grade school through young adults in college will compete to develop new innovations in nutrition, health, and wellness that will protect and enrich the lives of families. |
Numerous industry studies both private and public have shown that the behavior of families can be impacted through the eyes and voices of the children. Their fresh perspective on how to impact childhood nutrition, health, and wellness through innovation can have terrific impact on the products, services, and technologies we may use in the future. Served by multi-generational innovation panels of children, young adults, industry leaders, seasoned innovators, and academics; the CareKids program is focused on global problems that can be solved locally. |
|
|
||||||
|
|
High Performance Imaging Programs: |
|
Overuse and misuse of imaging studies is a global problem that leads to excessive radiation exposure and incidental findings that generate healthcare harm and cost. Underuse of studies due to the fear of radiation exposure can lead to missed and delayed diagnoses. There are 240 million CT scans undertaken worldwide and 80 million in the USA. Ten percent are done on children, and technically at least half of these are "imaging accidents" where better quality could be delivered and or less radiation can be used.
|

|
|
Stephen J. Swensen, MD, MMM, FACR Dr. Swensen is the former Medical Director for Leadership and Organization Development. He has served as the Director for Quality and Associate Dean for Value. Read bio... Stephen J. Swensen, MD, MMM, FACR, is the former Medical Director for Leadership and Organization Development. He has served as the Director for Quality and Associate Dean for Value. He is Professor in the Mayo Clinic College of Medicine. Under his leadership the Quality Academy and the Value Creation System were established. In these programs, several thousand staff are trained each year. There are more than 13,000 certified Bronze, Silver, and Gold Quality Fellows. Dr. Swensen chaired the Department of Radiology from 1998-2006. His leadership team used Lean-Sigma and Baldrige methods to improve the value of care for patients provided by 1,200 staff, who performed more than one million exams annually. During his tenure the department was recognized as the #1 radiology practice in the country (Medical Imaging) and the most patient-centered (Diagnostic Imaging). He holds a Master of Medical Management degree from Carnegie Mellon University's Heinz School of Public Policy and Management. He received his MD from the University of Wisconsin. His residency training was at Mayo Clinic and his Thoracic Radiology Fellowship at Harvard Medical School, Brigham and Women's Hospital. Dr. Swensen is a member of the Institute for Healthcare Improvement faculty. He served as the healthcare member of The Conference Board’s U.S. Quality Council. He is past President of two international societies, the Fleischner Society and the Society of Thoracic Radiology. He chaired the American College of Radiology's Quality Metrics Committee and led the RSNA's Continuous Quality Improvement Initiative. He is a member of the AAMC Integrating Quality Steering Committee. He founded the Big Sky Quality Roundtable and the Keystone Quality Officer Group, and co-founded the Sun Valley Assembly. He has been Principal Investigator of three NIH grants related to lung cancer screening with CT and diffuse infiltrative lung disease. He has authored two books and more than 130 peer-reviewed articles. Hide bio |
Charles R. Denham, MD Dr. Denham is an international leader in patient safety and high-performance care solutions. He has taught and led research in medicine, engineering, and business leadership. Read bio... Dr. Denham is an international leader in patient safety and high-performance care solutions. He has taught and led research in medicine, engineering, and business leadership. He is involved in coordinating U.S. and international quality, certifying, and purchasing organizations along a path of harmonization of measures, standards, and practices, which encourages hospitals and healthcare organizations to dramatically improve patient safety and care performance. He co-chairs the U.S.-based National Quality Forum group that annually updates the NQF-Endorsed® Safe Practices for Better Healthcare, which are increasingly being tied to value-based purchasing. He chairs the Leapfrog Group Safe Practices Program, which influences more than $69 billion in purchasing power. He is Chairman of TMIT, which operates a national research test bed of more than 3,100 hospitals, through which it pursues its mission of "saving lives, saving money, and building value in the communities served." Dr. Denham is a Senior Fellow of the Harvard Advanced Leadership Initiative, and has a faculty appointment at the Harvard School of Public Health. He is an Adjunct Professor at the Mayo Clinic College of Medicine in Healthcare Engineering. He is the Editor-in-Chief of the Journal of Patient Safety and a co-founder of the Global Patient Safety Forum. Hide bio |
|||
|
J. Michael Henderson, MD Dr. Henderson is Chief Medical Officer at the University of Mississippi Medical Center and the former Chief Quality Officer at the Cleveland Clinic. His interest in quality was initially triggered in the surgical arena, implementing standardized approaches to preoperative processes, and becoming a champion... Read bio... J. Michael Henderson, MD, is Chief Medical Officer at the University of Mississippi Medical Center and the former Chief Quality Officer at the Cleveland Clinic. His interest in quality was initially triggered in the surgical arena, implementing standardized approaches to preoperative processes, and becoming a champion for the National Surgical Quality Improvement Program of the American College of Surgeons. In 2005, he embarked on an expansion of Quality and Patient Safety for the Cleveland Clinic. His leadership support in establishing the Quality and Patient Safety Institute has provided a central coordinating quality focus across the more than 20,000 employees. This Institute collaborates with the clinical and support departments to align quality outcomes and patient safety into daily practice for the entire healthcare team. The focus of this work is to make daily practice patient-centric, clinically relevant, operationally effective, regulatory compliant, and academically appealing. Hide bio |
Edward Kelley, PhD Edward Kelley, PhD, currently serves as Coordinator and Head of Strategic Programmes for WHO Patient Safety. His responsibilities include the development of new programmes and partnerships... Read bio... Edward Kelley, PhD, currently serves as Coordinator and Head of Strategic Programmes for WHO Patient Safety. His responsibilities include the development of new programmes and partnerships, oversight of WHO Patient Safety presence in London and Baltimore and leadership on several key programmes within WHO Patient Safety. Prior to joining WHO, Dr. Kelley directed the only ongoing national examination of healthcare quality and disparities in the United States as the Director of the U.S. National Healthcare Reports for the U.S. Department of Health and Human Services in the Agency for Healthcare Research and Quality (AHRQ). These reports track levels and changes in quality of care for the American healthcare system at the national and state level, as well as disparities in quality and access across priority populations. Hide bio |
|||
Surfing the Healthcare Tsunami: Bring Your Best Board™
| TMIT is producing inspiring multimedia stories to drive high performance care and improve patient safety in hospitals by showcasing great role models – emphasizing the positive rather than the negative. Stories igniting hope and faith will include those told by consumers, front-line caregivers, clinical and non-clinical leaders of hospitals, and international subject matter experts. | Certain broadcast programs will be shown globally, and then will be made available to hospital leadership, front-line performance teams, and consumers. The series of "arc to action" stories will be told to inspire both consumers in communities and hospital leaders to act locally. | ||
Play HD documentary below. Please note: best viewed in full screen mode.
|
|||
Chasing Zero: Winning the War on Healthcare Harm
Play HD documentary below. Please note: best viewed in full screen mode.
|
|||||||